Epilepsy is a central nervous system disorder characterized by abnormal brain activity, causing seizures or periods of unusual behaviour, sensations and sometimes loss of awareness. It is one of the most common neurological diseases globally.
Epilepsy is a chronic non- communicable disease of the brain that can affect males or females of all races, ethnic backgrounds and races. Seizures are a brief episodes of involuntary movement that may involve a part of the body or the entire body.
Seizures can be classified into two main groups:
Generalized & Focal Seizures
1. GENERALIZED SEIZURES affect both sides of the brain and can further have 2 sub-types:
– Absence Seizures or Petit Mal Seizures cause rapid blinking or staring into space for a few seconds.
– Atonic Seizures or Drop Seizures cause a loss of muscle control especially the legs causing you to suddenly collapse or fall down.
– Tonic-colonic seizures or Grand Mal Seizures cause a person to cry out, make them unconscious abruptly, fall to the ground or even have muscle jerks or spasms.
2. FOCAL SEIZURES or PARTIAL SEIZURES can affect just one area of the brain.
– Simple focal seizures cause twitching or a change in sensation by affecting a small part of the brain.
– Complex focal seizures can cause confusion or daze making a person unable to think and react properly for up to a few minutes.
– Secondary generalized seizures begin affecting one part of the brain, spreading to both sides later on. In other words, a focal seizure developing into a generalized seizure.
How Common is Epilepsy?
1. As per World Health Organization (WHO), around 50 million people worldwide have epilepsy.
2. A study published in the journal EPILEPSIA “Prevalence and pattern of epilepsy in India”, predicts that there are more than 10 million persons with epilepsy (PWE) in India with a prevalence of about 1% in Indian population.
3. Just about 80% of people with this condition live in low- and middle-income countries.
4. Around 75% PWE living in low-income countries do not receive suitable treatment.
5. An appropriate diagnosis and treatment can help about 70% PWE lead a seizure free life.
6. PWE are at a three times higher risk of premature death than the general population.
7. PWE and their families face a lot of stigma and discrimination around the world.
8. WHO says that around 25% epilepsy cases are preventable.
Epilepsy Management
Treatment of epilepsy includes anti-seizure medications, special diets (typically in addition with anti-seizure medications) and surgery.
1. Medications: Certain medicines called Anti-seizure drugs (anti-epileptic medicine) are accessible which limit the spread of seizures in the brain. The success rate of anti-seizure medicines is about 2 in 3 people with epilepsy. A combination of these medications can help decrease the frequency and intensity of seizures.
2. Surgery: Epilepsy surgery is a treatment method of choice in people with focal seizures, mostly when the seizure focus is located in the temporal lobe of the brain and secondly when doesn’t interfere with vital functions such as speech, language, motor function, vision or hearing. Surgery either help to stop future seizures or make them easier to control with medicine.
3. Diet: Some people with epilepsy especially children, have been able to reduce their seizures by following a strict diet regime namely Ketogenic Diet, which is high in fats and low in carbohydrates. It can be a challenge and must be done under medical supervision.
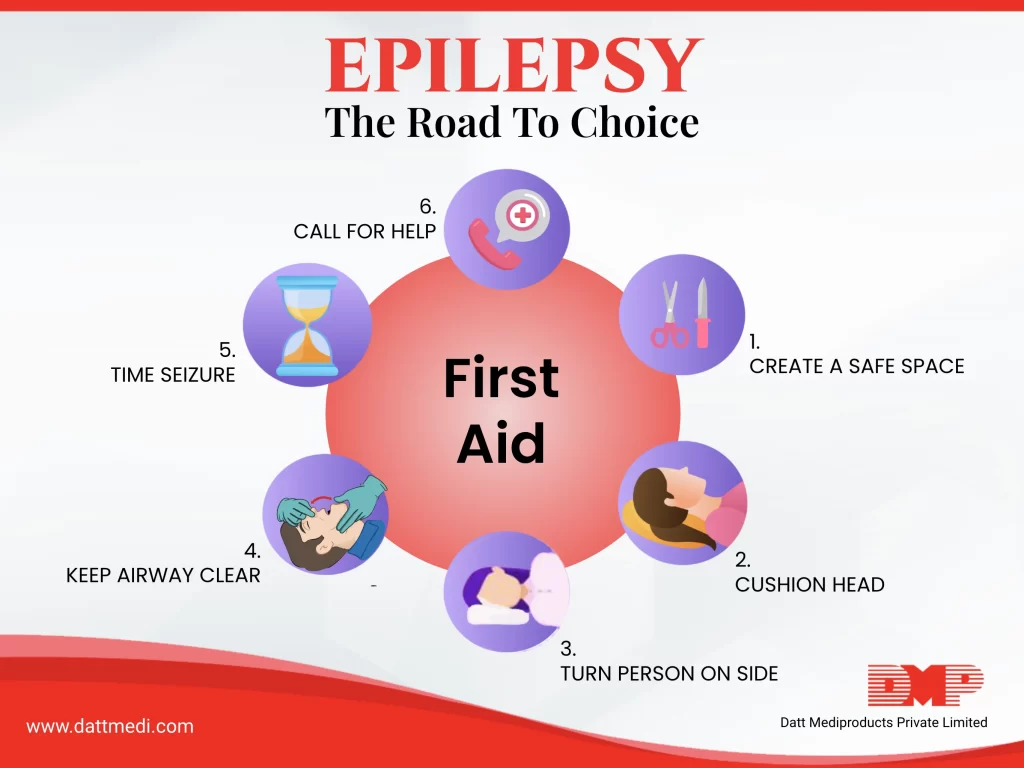
SEIZURE FIRST AID
Apart from the above management techniques, there are certain steps involved in Epilepsy Seizure First Aid to help someone having a seizure.
Step 1: Create a Safe Space: Keep the person safe from harm. Move away any hard objects from the area to protect them from injury.
Step 2: Cushion Head: Put something soft and small under their head.
Step 3: Turn Person on Side if they are not awake and aware or if they have food, fluid or vomit in their mouth.
Step 4: Keep Airway Clear: Loosen tight clothes around neck and keep the airway clear.
Step 5: Time Seizure: Check the time and call an ambulance if the seizure lasts for a longer than 5 minutes or if the person doesn’t return to their usual state.
We recommend staying with the person until seizure ends and comfort them when they regain consciousness. Do not put any objects in their mouth and give rescue medicines only if prescribed by a health care professional.
Follow us @dattmediproducts or visit www.dattmedi.com for more health related information.
Stay updated, Stay Healthy!