A Stroke is defined as an abrupt death of brain cells. This is caused by the blockage of blood vessels which supply blood, oxygen, and nutrients to the brain. Because of this interrupted blood supply, the brain cells begin to die.
A stroke is the 5th leading cause of death in the US. According to the American Heart Association (AHA), African-Americans are at a much higher risk of death from stroke.
A stroke is a medical emergency which needs to be diagnosed and treated at the earliest to reduce brain damage and to prevent further complications. Different types of strokes may have a different lines of treatment.
Let us understand the different types of strokes:
TYPES OF STROKE
1. Ischemic Stroke (Clots)
An Ischemic stroke occurs when the blood supply is disrupted to a region of the brain because of blockage in the artery supplying blood to the brain caused either by the blood clots or by artery blockage. This type of stroke accounts for 80-90% of all strokes and is the most common type of stroke.
2. Hemorrhagic Stroke (Bleeds)
This stroke occurs when a weakened blood vessel ruptures. The blood spill creates swelling and pressure and damages the brain cells & tissues. This type of stroke is less common and accounts for 15% of all strokes and but is responsible for 40% of all stroke deaths.
3. TIA (Transient Ischemic Attack)
This is similar to the Ischemic stroke in which blood supply to a brain part is disrupted but this is for a short while. TIA is a reversible stroke and the symptoms disappear within 24 hours. This is a silent stroke and a warning signal for future strokes and should be taken seriously. A transient ischemic attack is also called as Reversible Ischemic Neurological Deficit (RIND).
4. Cryptogenic Stroke
A stroke with an unknown cause is called a “cryptogenic stroke.” The event is transitory or reversible and the cause is truly unknown. This is more common in younger patients than in older patients.
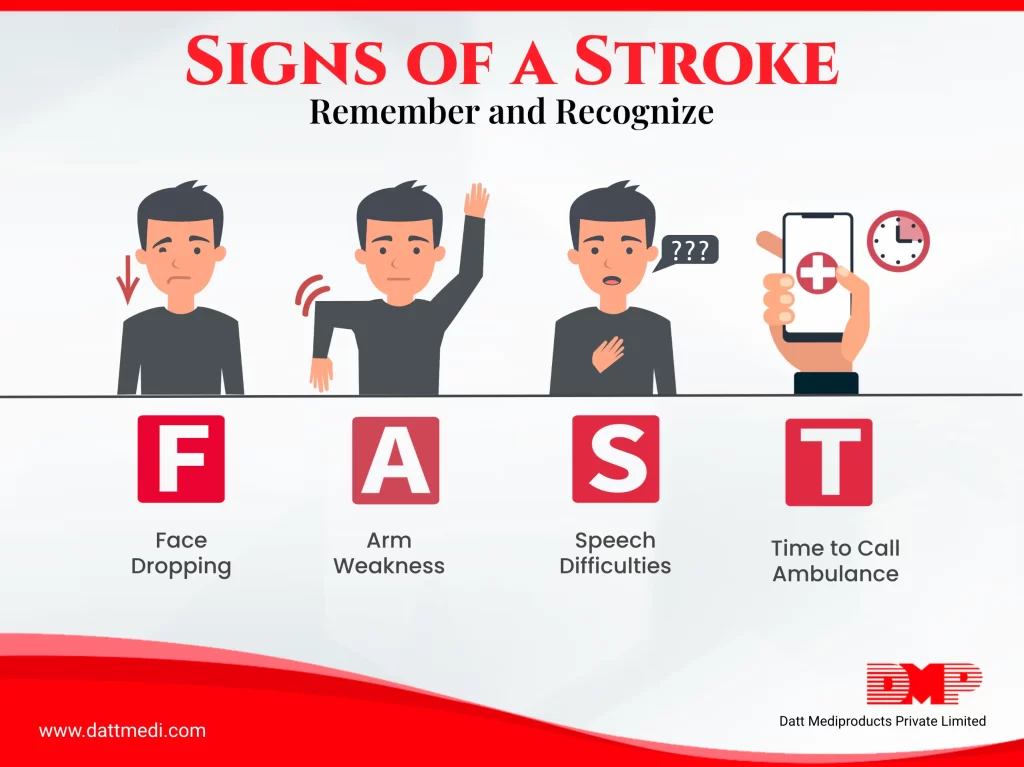
Spot a Stroke with these 4 key symptoms (F.A.S.T):
- FACE DROOPING: When one side of the face becomes numb or droops. Ask the person to smile and see if the smile is uneven.
- ARM WEAKNESS: Ask the person to raise both the arms and see if one of the arms drifts downwards.
- SPEECH DIFFICULTIES: Slurred speech or dysarthria (Difficulty in speaking or understanding).
- TIME TO CALL AMBULANCE: If the person is positive for any of these symptoms, rush and call the ambulance and seek doctor’s advice immediately.
Following are a few additional signs of a stroke:
- Numbness: Sudden numbness in the limbs especially on one side of the body.
- Confusion: Any sudden confusion, difficulty in speaking or understanding speech.
- Trouble Seeing: Vision loss in one or both the eyes.
- Trouble Walking: Sudden trouble in walking, dizziness, and loss of balance.
- Severe Headache: Sudden severe headache with an unknown cause.
80 % of the strokes can be prevented.
Some healthy lifestyle changes are recommended to prevent stroke, which might seem similar to the ones involved in heart disease.
– Keeping a check on high blood pressure
– Lowering the cholesterol levels, trans fats and saturated fats in the diet
– Consuming a healthier diet including high proteins, vegetables, fruits, grains, low fat or fat-free dairy products
– Exercising regularly and losing weight to help reduce blood pressure
– Quitting smoking, tobacco, etc. Do you know smokers are at double risk of stroke than the non-smokers?
– Limit alcohol use as it has been linked to stroke in many studies.
A Stroke is a medical emergency and swift action is critical as it can help reduce the damage and prevent further complications. We @ Datt Mediproducts understand the complexity of the situation and recommend seeing a doctor immediately after a positive test of F.A.S.T., brain damage can be highly reduced and life can be saved.




