Blood Donation is the process of voluntarily donating blood to save people who are ill or injured, or who need blood for any other medical need. Blood is screened for easily transmittable diseases like AIDS, Syphilis, and viral hepatitis.
Then, it can be transfused whole or separated into its different components; for example, red blood cells, plasma or platelets and used as per the needs of the recipient.
SOME FACTS Every year June 14th is observed as “World Blood Donation Day” India requires about 4-5 crore units of blood every year, out of which only a meager percentage is available. As per WHO, there is an annual deficit of 2 million units of blood in India. Only 1% of the Indian population donates blood every year “Type O-” is a universal donor and as a result it is the most requested blood group Up to 100 units of blood may be required by a single car accident victim Apheresis is the process in which the donor is hooked up to a machine that can help collect and separate the different blood components.
Each unit of donated blood can be separated into 4 different components and can save multiple lives:
– RBCs can be used for trauma, surgical and anemic patients or post-delivery.
– Plasma can be administered to patients with clotting issues.
– Platelets are often used in cancer, and transplant patients.
Who can be a Donor?
– The minimum age for blood donation is 18 years.
– Minimum body weight is 50 kg. A donor should not be underweight.
– A donor should not suffer from any infections or chronic diseases like Diabetes, Flu, AIDS.
– A donor should have a healthy iron level.
– A donor should have normal blood pressure.
– A donor should not be pregnant or menstruating.
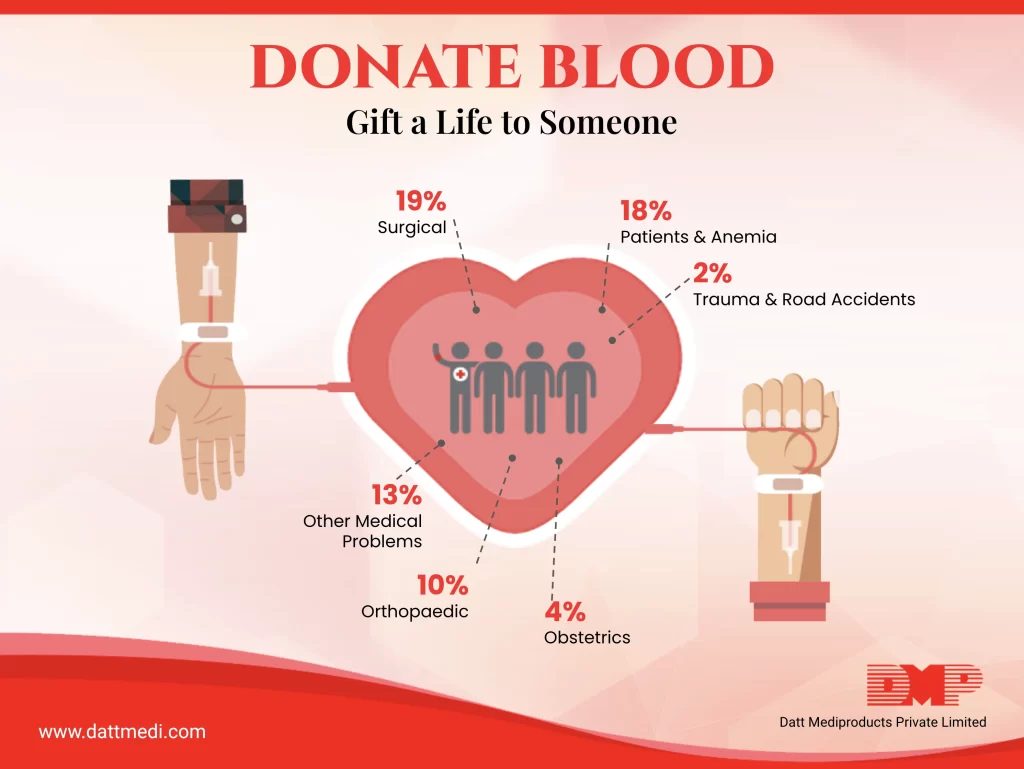
Who needs a blood transfusion?
– Patients with Anemia, Sickle Cell Disease, Thalassemia
– Patients suffering from bleeding disorders like Hemophilia
– Patients undergoing surgery need a blood transfusion to replace any blood loss during their surgery.
– Cancer patients
– Trauma & Burn Victims
– Acute kidney failure patients
– Immune System Disorders
– Females post delivery
Donating blood can be beneficial for your Physical and Mental Health.
Donating blood is good for your heart:
It reduces the blood’s viscosity level; lowering the risk of a heart attack and/or other heart diseases. This has been proved in a study published in the Journal of Blood Medicine “Lipid Profile of Regular Blood Donors”, stating that a regular blood donation significantly lowers low-density lipoproteins and mean total cholesterol.
Donating blood lowers your blood pressure:
A 2016 study published in the journal “Transfusion” shows that regular blood donation helped in reducing blood pressure in hypertensive individuals.
Donating blood reduces iron levels:
Iron is an important mineral for producing RBCs. But too much iron can be harmful also, as it may deposit in different organs like heart and liver affecting their functions. This condition is known as “Hemochromatosis” or “Iron Overload”. Donating blood has been proven to be beneficial in lowering iron stores and preventing hemochromatosis, liver damage, cirrhosis, heart abnormalities etc.
In India, several organizations are involved in organizing blood donation camps and raising awareness of the benefits of donating blood. Donors can register with such organizations like Indian Red Cross Society, Rotary Blood Bank, Think Foundation, etc.
We @ Datt Mediproducts encourage healthy and active individuals to donate blood regularly. As your one donation can save as many as three lives.
So, Donate Blood because there is no Substitute to it!