We may agree that we all need to drink an average of 8 glasses of water per day. But we all may not be aware that it depends upon various factors like our gender, age, activity levels, and external environment.
When we exercise, more water is excreted through perspiration. Hence, water requirement increases. On the other hand, requirement decreases as we age. Water is vital to the body’s normal functioning.
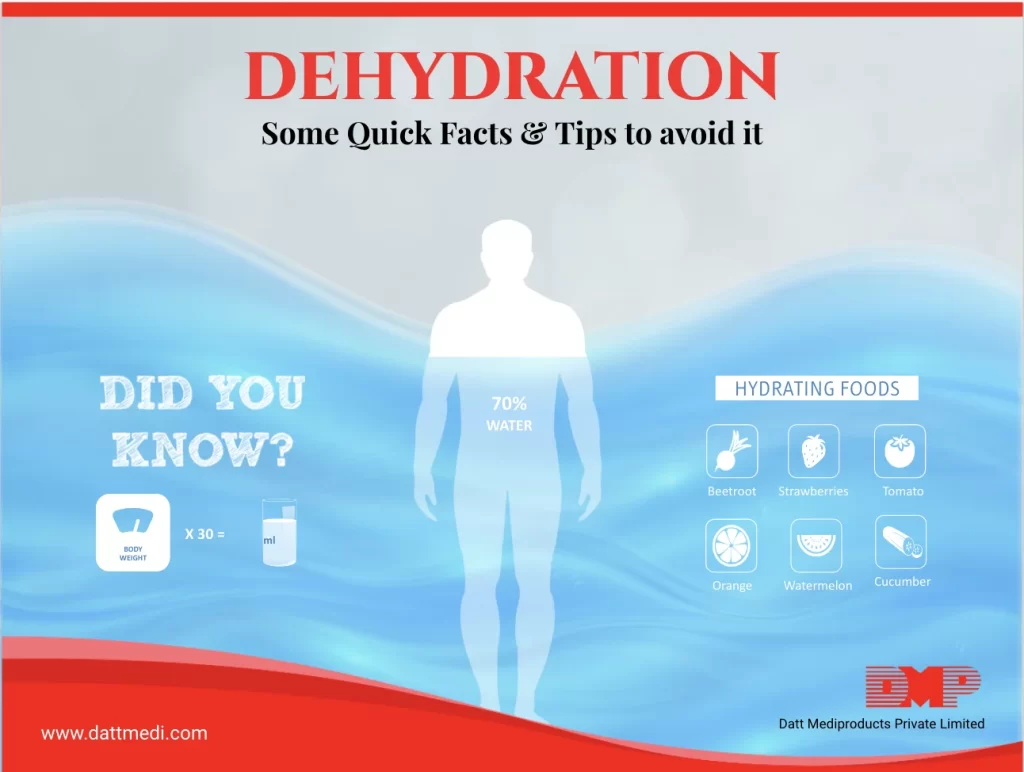
Adequate water intake of 30 ml/kg body weight is recommended in a person with normal functioning kidneys and heart, as documented in the Indian Journal of Clinical Practice, Vol. 22, No. 12, May 2012.
We lose water when we sweat, pass urine or exhale. Water may also be lost in a few pathological conditions like diarrhea and vomiting. When this loss water is not compensated, it leads to dehydration. Dorland’s Illustrated Medical Dictionary defines “Dehydration as the condition that results from excessive loss of body water”.
Dehydration can become serious if not treated. When water between 10-15% of the body weight is lost, it can also lead to seizures and unconsciousness. Untreated dehydration causing water loss of >15% of body weight might result in brain damage and ultimately death.
Some Quick Facts: 1. 75% of the human body is water. 2. Dehydration results when water intake is less than water loss. 3. Dehydration may be caused by diarrhea, vomiting, high fever, excessive sweating, increased sweating or heat waves. 4. Dry mouth, lethargy, tiredness, dizziness, dark-colored & strong-smelling urine may be the early signs of dehydration. 5. Babies, infants, old age people, athletes are more susceptible to dehydration. 6. While severe dehydration needs immediate medical treatment, mild to moderate dehydration may be reversed by drinking more fluids.
Symptoms:
Thirst is a reliable indicator that your body needs water. There are other important and distinctive symptoms of dehydration which may differ as per your age group.
Below are some of these symptoms:
|
Infants & Babies |
Adults |
|
Dry mouth and tongue Few or no tears when crying No wet diapers for three hours Sunken eyes & cheeks Sunken soft spot (fontanelle) Irritability |
Extreme thirst Less frequent urination Dark-colored urine Fatigue Lightheaded & Dizziness Confusion Palpitation & Rapid Heartbeat |
In case of severe malnutrition, dehydration may be caused by an untreated diarrheal disease leading to loss of water, fluids, and electrolytes. It may be difficult to identify dehydration in such cases because the indicators like skin elasticity may not be reliable. Others symptoms might include thirst, tiredness, weak radial pulse, and reduced or absent urine flow.
Few Tips to reduce the risk of Dehydration:
– Increase fluids intake when you sense any symptom of dehydration. It should be done gradually.
– Drink more fluids during the day time.
– Infants and Babies should be fed with a spoon making it easier to swallow the fluids.
– A pale clear pee color is an indicator of enough fluid consumption.
– People who are at high risk of dehydrating, like athletes and people who work outdoors, should drink more fluids.
– ORS may be consumed if you have diarrhea and your body is losing a lot of fluids.
– Fruit juices and fizzy drinks must be avoided for children. It may worsen diarrhea and vomiting.
It’s important to drink water and other fluids, eat seasonal juicy vegetables; especially during hot summer days and during illness. We understand that most occurrences of dehydration may be reversed by increasing fluids consumption, but severe dehydration needs immediate medical attention.
We @ Datt Mediproducts understand the Dehydration has an easy antidote but is potentially life-threatening if left untreated. So take good care!