Thyroid dysfunction doesn’t cause Diabetes and Diabetes doesn’t cause a Thyroid dysfunction. But both have an intersecting underlying pathology. The pathophysiological association between the two conditions has been attributed to the complex intertwining biochemical, genetic, and hormonal functions.
In the study titled “Frequency of thyroid dysfunction in diabetic patients: the value of annual screening”, published in the “Diabetic Medicine: a journal of the British Diabetic Association”, the prevalence of thyroid disorder in the diabetic population was documented.
The prevalence was reported to be 13.4% with higher prevalence (31.4%) in female T2DM patients as compared to (6.9%) in male T2DM patients.
Let’s see how both are related to each other.
How Thyroid Affects Diabetes?
The Thyroid has an important role in the body’s metabolism thus it affects diabetes also. It might not be easy to control diabetes in an individual with thyroid dysfunction.
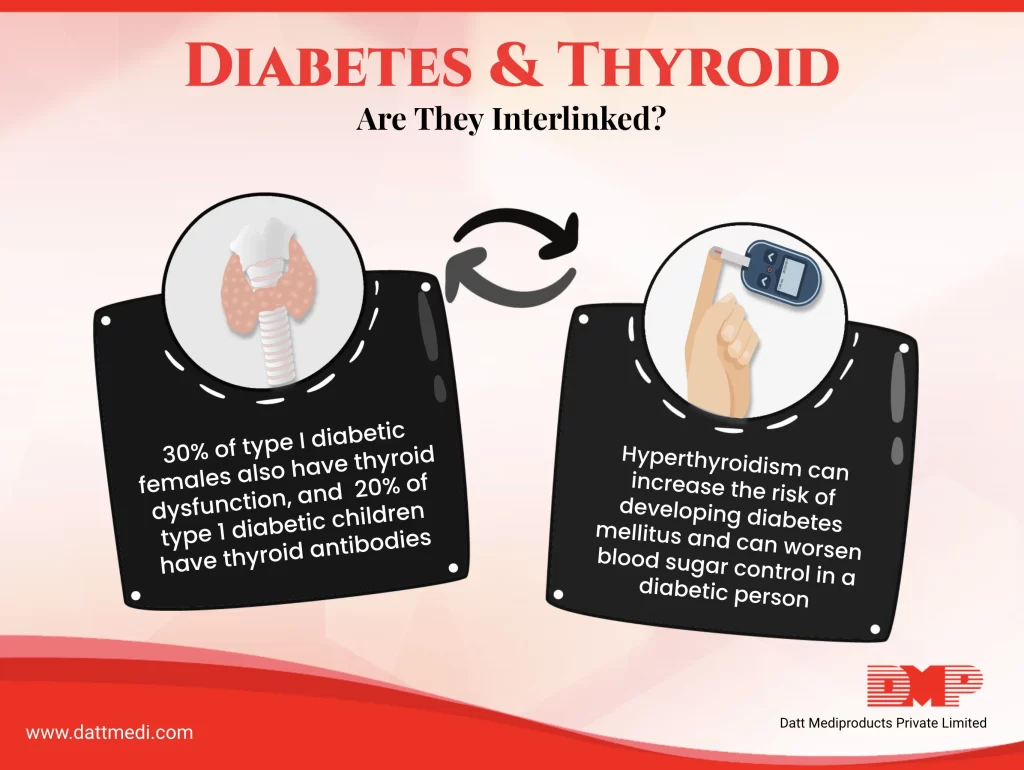
For example, in the case of hyperthyroidism, there will be elevated blood glucose levels because our body will use insulin much faster. As a result of increased levels of thyroid, the body metabolism will also increase affecting some important body functions like elevating the intestinal glucose absorption, hepatic glucose output, increased fasting & postprandial insulin levels and increased peripheral glucose transport accompanied by glucose utilization.
Similarly, when thyroid levels are low, insulin will be used at a much slower rate. The patient may have increased cholesterol, LDL and triglycerides, which may increase the risk of heart diseases.
INSULIN RESISTANCE
Thyroid dysfunction has been found to be associated with Insulin resistance, which has been reported to be the major cause of impaired glucose metabolism in T2DM. Hypothyroidism leads to decreased metabolism affecting nearly all major body functions like reduced glucose absorption from the gastrointestinal tract, diminished hepatic glucose output and reduced disposal of glucose. The reduced insulin synthesis subsequently leads to Hypoglycemia.
The role of thyroid dysfunction as a concurrent disorder of Type 2 Diabetes Mellitus (T2DM) has been evidenced by a number of preclinical, molecular, and clinical studies.
As per a study titled “Hypothyroidism Is a Risk Factor for New-Onset Diabetes: A Cohort Study”, published in the journal “Diabetes Care”, it has been concluded that Hypothyroidism is a risk factor for Type 2 Diabetes and identifying & treating Hypothyroidism might reduce the risk of Diabetes Mellitus (DM).
AUTOIMMUNITY
Autoimmunity has been seen as the major cause of the thyroid malfunction associated with diabetes. Type 1 Diabetes is an autoimmune disease and most of hypothyroidism is autoimmune as well. It has been implicated that if an individual has one type of autoimmune condition, they are more likely to have multiple autoimmune diseases.
Fact: 1 in 3 females suffering from Type 1 Diabetes have a chance of developing thyroid disorder.
During this Thyroid Awareness month, we @ Datt Mediproducts are creating awareness among the individuals about the link between Thyroid disease and Diabetes. We recommend seeing a doctor immediately when screened with thyroid disease and get treated. Screening is important as an undiagnosed and untreated thyroid disease may put patients at risk of certain serious conditions, such as cardiovascular diseases, osteoporosis, and infertility.