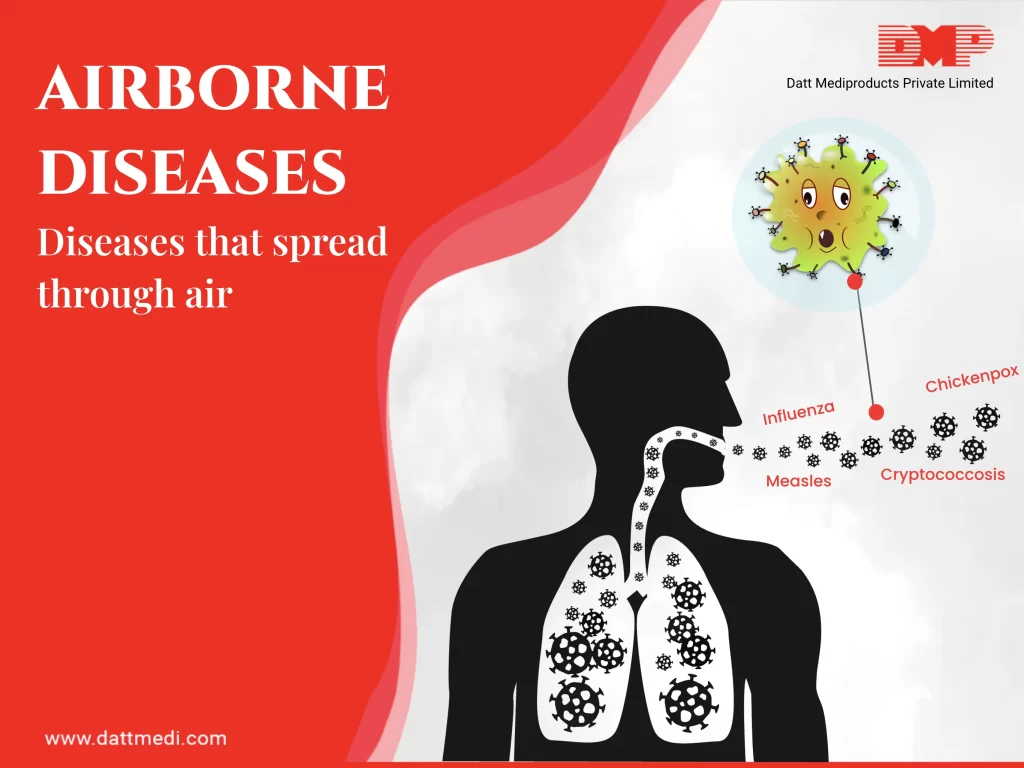
Airborne diseases are those, which are caused by microorganisms and spread through the air. These are mostly caused by pathogens like bacteria, fungi or viruses and are expelled into the air due to coughing, sneezing or talking.
Climatic factors such as humid conditions and persistently high temperature might also increase the risk of contracting airborne diseases. High humidity levels promote aerosol growth and deposition in the respiratory tract. On the other hand, loss of water is the greatest environmental stressor for the microorganisms to stay viable.
Several treatment options are available which we should know along with prevention techniques to avoid catching such diseases. We bring to you some facts about these airborne diseases and preventive measures.
SOME KEY POINTS:
1. Colds & Flu are airborne
2. Bacteria are transmitted through tiny pathogens in the air while coughing, sneezing or even talking
3. An airborne disease is contracted when someone breathes in the infected air
4. Symptoms that may range from mild to sever include: cough, chill, sneezing, runny nose, muscle or body aches, congestion, fatigue, etc.
5. Wearing masks and maximizing ventilation are good preventive options
6. Pregnant females, those undergoing cancer treatment, immunocompromised patients are more susceptible to airborne diseases
FEW AIRBORNE DISEASES:
Pathogens that cause airborne diseases cling to dust particles, moisture droplets, pollens, etc. These are picked up while breathing or through body fluids like mucus and phlegm. The disease-causing microorganisms multiply once inside your body.
Some common airborne diseases may include:
-Common cold
-Influenza caused by rhinovirus
-Varicella zoster (a virus which causes chickenpox in children)
-Mumps (virus attacks the glans beneath ears and even causes loss of hearing)
-Measles,
-Whooping cough or pertussis (caused by a bacterial infection and should be treated with antibiotics to prevent damage)
Some uncommon airborne diseases include:
-Anthrax
-Diphtheria
-Meningitis
PREVENTING AIRBORNE DISEASES:
Role of Proper Ventilation:
Poor ventilation (for example in overcrowded places) contribute to the spread of the disease, as disease-causing microorganisms, pollutants and moisture may build up to unsafe levels by decreasing the number of air exchanges.
Even a poorly maintained air-conditioning system may lead to the transmission of tuberculosis and legionellosis causing microorganisms as they build up in poorly ventilated areas increasing the transmission risk. Natural ventilation is an effective method for promoting infection control. Increasing ventilation helps the proper exchange of air thus diluting the contaminated air to reduce airborne infection rates.
Good Hygiene Practices:
Following good hygienic and sanitary habits help to reduce the risk of disease transmission. Regular hand washing, wearing a hospital mask in public places and covering your mouth while coughing or sneezing are some habits that are recommended.
Now that we have understood that these airborne diseases spread by cross contamination while an infected person coughs, sneezes or even talks, we @ Datt Mediproducts recommend following the required preventive measures so that the risk of contracting airborne diseases can be reduced.