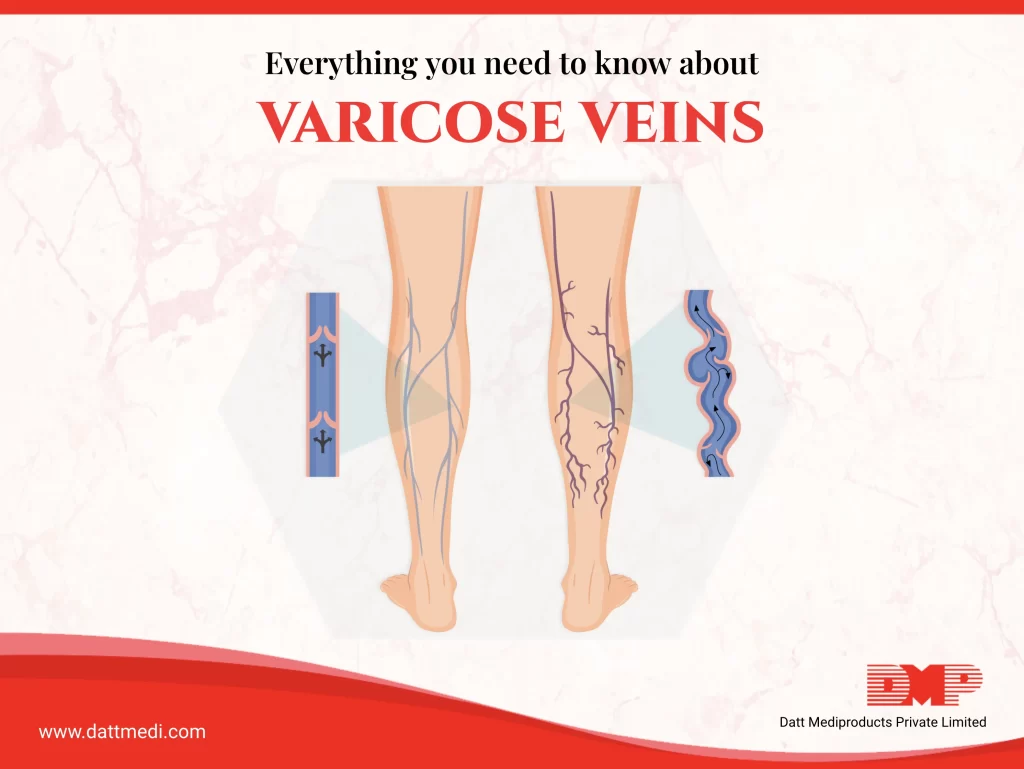
Varicose veins are enlarged, swollen, twisted veins ,often appearing as bulging, that can be seen just under the skin and are usually blue or dark purple in colour. They typically appear in legs but can affect other parts of the body too. Many people can have a mild version of varicose veins that can cause discomfort to the patient but sometimes it can lead to further more serious problems.
DO YOU KNOW-
Reports indicate that about 2%-73% of the global population is affected by varicose veins. However, varicose veins are a common condition in India, with an estimated 37.25% prevalence rate among the adult population.
What Causes Varicose Veins?
Varicose veins occur in the superficial veins and can be caused by an increased blood pressure in the veins. Our veins have one-way valves that open and close to ensure the blood flowing towards the heart. When these valves become weaken or damaged, the blood collects in the veins or even flows backwards. This causes veins to grow larger and become distorted, thereby resulting in varicose veins.
Symptoms:
- Bulging, twisted, swollen, bluish vein or veins
- Swelling in the legs
- Sensations in the legs, such as a heaviness, burning, and/or aching pain
- Rash or Itching around the vein or veins
- Skin colour changes around the vein or veins
- Night time leg cramps
Sitting or standing for long periods can cause the blood to pool which may worsen the symptoms. Lying down and putting feet up at elevated position may help you get better.
How does stockings help?
Compression stockings are designed to provide consistent pressure in the legs to prevent swelling and help improve circulation. Compression therapy may be recommended as a treatment or after a procedure to remove or close off varicose veins.
Compression therapy helps relieves symptoms of varicose veins. These also help heal leg ulcers or sores that are a complication of varicose veins. Because the problem is long term, doctors may suggest wearing compression stockings for a long period of time.
As per a 2018 study titled “Acute Effects of Graduated Elastic Compression Stockings in Patients with Symptomatic Varicose Veins: A Randomised Double Blind Placebo Controlled Trial” published in the journal “European Journal of Vascular and Endovascular Surgery”, wearing compression stockings with pressures of 18 to 21 millimetres of mercury (mm Hg) for 1 week helped to reduce aches and pain associated with varicose veins, compared to normal stockings.
VELCARE® – Varicose Veins Stocking
It is a varicose veins medical compression stockings which provides therapeutic graduated compression between 23-32mmHg, a class 2 compression. The stockings are very soft, latex free, breathable and designed to offer optimal comfort to the user. Velcare® stockings are highly durable and offer a four-way stretch. Using these compression stockings helps blood circulation from lower sides to upper sides.
Indicated in the management of Deep Vein thrombosis, these stockings can also be used to treat Phlebitis & are optimal for postoperative care. Velcare® Stockings work excellently to relieve leg swelling, moderate to severe varicosities and oedema.
We, Datt Mediproducts understand that varicose veins may interfere with daily activities. Adopting certain lifestyle changes such as maintain a healthy weight, being physically active and avoiding standing or sitting for long periods can help relieve varicose veins symptoms or even prevent them from getting worse.
Keep moving & Stay Healthy!






