Varicose veins are enlarged, twisted veins that bulge under your skin. They normally develop when blood flow is obstructed and are more than just a cosmetic concern; they can cause discomfort and, if untreated, lead to more serious health issues. Medical compression stockings and wraps, such as the Velcare® range from us, provide an effective solution for managing varicose veins. Understanding their benefits and features can help you make an informed choice.
Velcare® Varicose Vein Stockings: Support Where You Need It
Designed to offer Class 2 Compression (23-32mmHg), Velcare® Varicose Vein Stockings are ideal for promoting circulation and reducing varicose vein symptoms. The graduated compression applies gentle pressure from the ankle upwards, aiding blood flow back to the heart.
Key Features of Velcare® Varicose Vein Stockings:
1. Effective Compression: Reduces swelling and discomfort associated with varicose veins.
2. Comfortable Wear: Soft, breathable, latex-free materials ensure all-day comfort.
3. Durable Construction: Four-way stretchability enhances flexibility and durability for long-term use.
4. Medical Grade Quality: Designed to meet medical standards for effective varicose vein management.
Velcare® Inelastic Wrap: Customizable Compression
For those preferring an alternative to traditional stockings, Velcare® Inelastic Wrap provides targeted calf compression without constant adjustment. Adjustable straps offer a customized fit for optimal compression therapy tailored to individual needs.
Key Features of Velcare® Inelastic Wrap:
1. Targeted Compression: Focuses on calf muscles for effective circulation support.
2. Adjustable Fit: Velcro straps ensure a secure fit and ease of adjustment.
3. Ease of Use: Simple application and removal for convenient daily wear.
4. Breathable Material: Allows the skin to breathe, suitable for extended use.
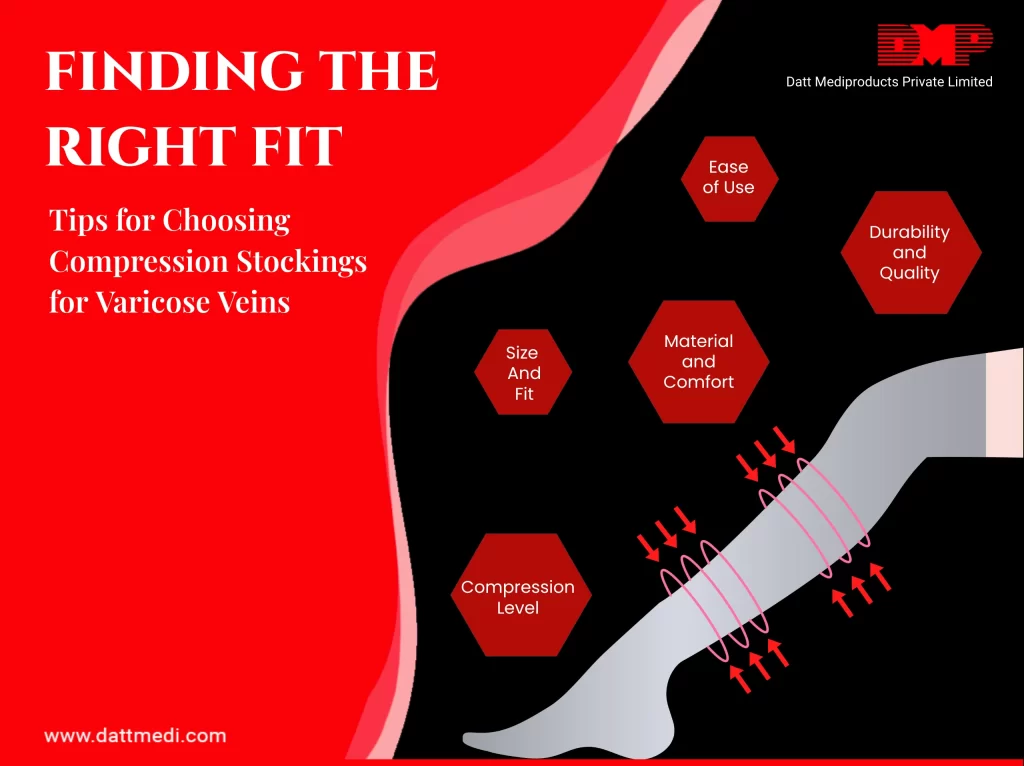
Choosing the Right Option for You
When deciding between Velcare® Varicose Vein Stockings and Velcare® Inelastic Wrap, consider your lifestyle, comfort preferences, and specific medical needs. Both options offer effective relief for varicose veins, with the Stockings providing graduated compression and the Wrap offering targeted support and ease of use.
Whether you choose the graduated compression of Velcare® Varicose Vein Stockings or the targeted support of Velcare® Inelastic Wrap, we as Datt Mediproducts, ensures you receive high-quality products designed to improve circulation and alleviate varicose vein symptoms.
Explore more about Velcare® products and find the right solution for managing your varicose veins with us. For more information on our comprehensive range of wound care products – please visit www.dattmedi.com/wound-care.html