A Heat Stroke is a serious medical condition in which the body temperature rises above 40˚C and can’t cool down on its own. Any physical exertion in such hot conditions or the environment itself could cause a Heat Stroke.
The ultimate aim while treating a heat stroke patient is to cool the body temperature as early as possible and prevent further damage to other organs, otherwise, the condition can be fatal.
As per the Centers for Disease Control and Prevention (CDC) statistics published in 2012, as many as 7,415 people died as a result of Heat Stroke in the United States between 1999 and 2010. According to a report published by the National Institute of Disaster Management (India), 2016, the no. of heat deaths has been on a rise over the last two decades. Over these years, India has had no less than 393 deaths each year caused by heat waves and heat strokes.
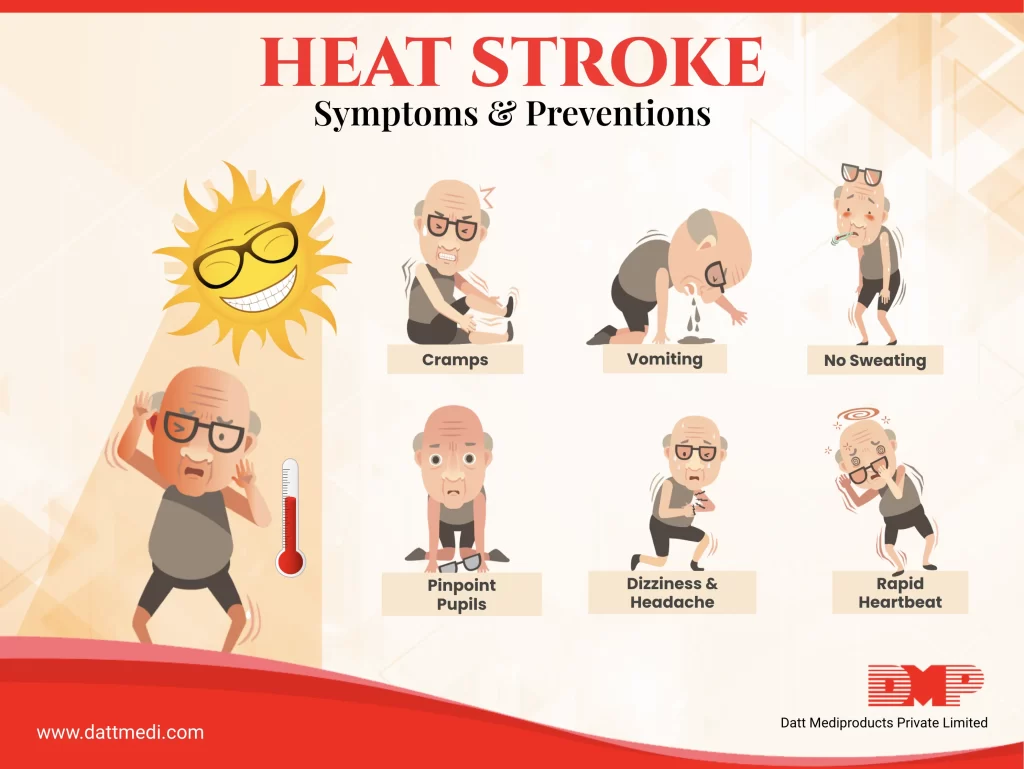
Following are the warning signs and symptoms of a Heat Stroke:
– High Body Temperature: Body temperature rising above 104˚F (40˚C) is the main characteristic sign of a heat stroke.
– Hot, red, dry or damp skin: Any alteration in sweating could be another sign of a heat stroke. The skin may feel hot and dry if a heat stroke is caused by hot weather and may be moist if it is a result of physical exertion. The skin may turn red as the body temp. increases.
– Fast, strong pulse: A significant increase in the pulse rate due to the stress caused by the heat in order to lower the body temperature.
– Mental or Behavioral Changes: Changes at the mental level caused by a heat stroke may include confusion, seizures (in children), agitation, irritability, restlessness, slurred speech, hallucination, and coma.
– Headache: Extreme headaches and one would feel ones head throbbing.
– Shortness of breath: Breathing difficulties, the breath may become shallower and quicker.
– Excessive Thirst: If not treated immediately, a Heat Stroke may impair the vital body organs like brain, heart, kidney, and muscles.
Nausea & Losing Consciousness etc.
What can you do when you observe these symptoms?
A Heat Stroke is a medical emergency. Seeking a professional medical help immediately or calling an ambulance right away is beneficial for the patient.
You can also do the following in Heat Stroke:
- The person who has suffered a heat stroke must be moved to a cooler place preferably an air-conditioned environment.
- Make the person lie down with slightly raised feet.
- Assist the person to lower his/her body temperature by using wet towels or a cool bath or ice packs.
- Some drinks like ORS, lemon water or juice can be given to rehydrate. However, this point should be avoided in case the person is not conscious.
What can you do to prevent a Heat Stroke?
Heat Strokes can be predicted. The risk is high during hot weather and rigorous exercise sessions.
Adopting appropriate measures can help prevent heat strokes and other heat-related illnesses:
1. Clothing: Wearing lightweight, light-colored, loose-fitting clothing may help to prevent heat strokes as they allow the body to cool down properly.
2. Fluid Intake: Drink plenty of fluids to replenish the water and electrolytes lost due to sweating in hot weather or exercise. Do not wait to get thirsty. Stay away from alcohol and sugary drinks as these can cause stomach cramps.
3. Avoid Sunburns: Apply sunscreen generously, wear a hat and sunglasses while outdoors to avoid sunburn as it will affect your body’s ability to cool down on itself.
4. During Car Parking: It’s not safe to leave anyone, especially children in parked cars as its temperature may rise to 20˚F in 10 minutes itself.
5. Be Cautious: People who are at a high risk of being hit by a heat stroke, maybe because of their medical conditions, age, or medications, should avoid strenuous outdoor activities on hot days.
Limit the outdoor activities to the coolest hours of the day like morning and evening.
Heat Stroke is a potentially fatal condition. We @ Datt Mediproducts recommend consulting a doctor immediately when you feel extremely weak, dehydrated or sense vomiting, shortness of breath, or any change in the mental status and abnormal behaviour.
Stay Cool, Stay Hydrated!