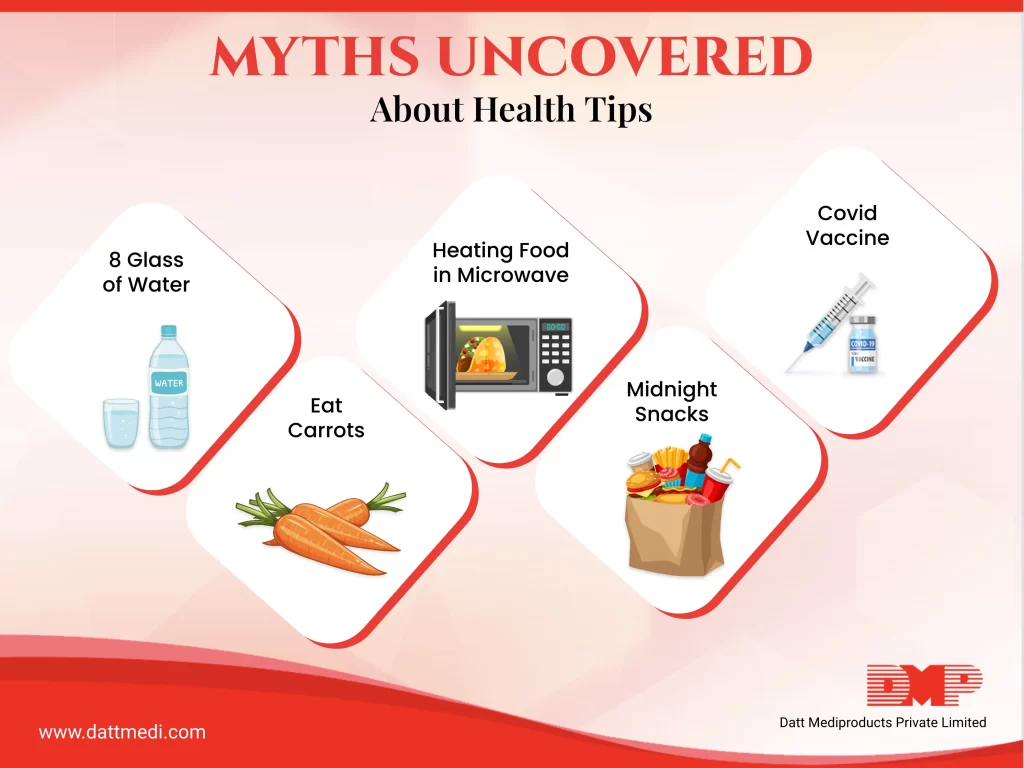
Eating sweets causes Diabetes; Mid-night snacking will lead to weight gain; Cooking food in microwave oven causes cancer.
Is this really true…. Science has unfolded some of the sayings that were passed on through ages.
Myth 1: Covid vaccine doesn’t work well
Fact: Vaccines are perhaps the best hope to tackle the adversity of Covid infection. It is a misconception that if we get vaccinated, then we won’t get infected. But the fact is that vaccination makes the illness less severe and reduces the risk of hospitalisation and death.
Myth 2: Eating too much sugar causes diabetes
Fact: Sugar does not cause diabetes. Having more sugar increases weight and being obese increases the chances for Type 2 Diabetes. Several other factors include physically inactive, family history and Insulin Resistance. Type 1 Diabetes is caused due to the faulty immune response when insulin-producing cells in pancreas are destroyed by our immune system so our pancreas stops being able to produce insulin. So, pay attention to diet and overcome sedentary lifestyle.
Myth 3: Using public toilet causes UTI
Fact: Urinary Tract Infections (UTI) are common in women. We, women are very paranoid of using public toilets, as these are home to lots of germs like E. coli, Staphylococci and many more. But the fact is that germs cannot be transmitted as they cannot survive for long time on the seat.
Some of the major causes of UTI are menopause, unhygienic sexual practice, holding back the urge to urinate, urinary catheters in case of hospitalization.
However, for personal hygiene it is suggested to carry a toilet seat sanitizer, or disposable toilet seat covers along to be at mental peace.
Myth 4: Cracking knuckles causes Arthritis
Fact: People who don’t crack knuckles and the habitual knuckle crackers both are at equal risk of arthritis. Cracking knuckles may only annoy people around but it won’t raise the risk for arthritis.
Myth 5: Midnight snacking increases weight
Fact: The key player that contributes to weight gain is net calorie intake (Calories consumed – Calories burnt) and not the time when we eat.
If you stay within body’s daily calorie limit, then night time eating does not actually lead to weight gain. However, it has been observed that people who eat late-night are inclined towards high-calorie packaged food which otherwise should be avoided.
It is advisable to eat food at least three to four hours before going to bed for the body to be able to digest what you have eaten. Eating spicy and fatty food at night leads to acid reflux and less time to balance out net calorie intake.
Myth 6: Heating food in microwave causes cancer
Fact: Microwaves are non-ionizing radiations. And the only non-ionizing radiations that causes cancer are UV Rays. Microwave ovens use microwave radiation to heat food, but this does not make food radioactive. And the technology behind is that the water molecules in the food vibrate and the food gets heated.
It is advisable to use glass containers to heat or cook food in Microwave and keep plastic wares at bay
Myth 7: 8 glass of water a day
Fact: It is always good to have enough water, but not everyone needs 8 glasses a day. This requirement varies from person to person basis their weight and age.
The body has a sophisticated regulatory system that monitors hydration and sends a message when you need to drink. Keeping oneself hydrated is more important than the count. The regular water threshold could be met by beverages, juices and the food that contain water.
Certain medical conditions like kidney stones, strenuous exercise, and climatic conditions are the decisive factors.
We @dattmediproducts feel that it’s good to be conscious but misinformation must be tackled head on. It is best to get expert opinions and not just follow what we read online. It is always suggested consulting a qualified health practitioner to seek information as per the medical conditions.




