Organ Donation is the practice of recovering healthy organs from either living or a deceased human being, referred to as a Donor, with the purpose of transplanting into a recipient. The process of recovering the organs from a donor is called retrieval.
Some Facts & Stats on Organ Donation:
– Organ Donation Day is observed on the 13th of August every year.
– The aim is to motivate healthy people to donate organs, and also to spread awareness about the importance of organ donation.
– As per a survey report mentioned on the National Health Portal (India), every year about 500,000 people die because of the non-availability of organs, 200,000 people die due to liver disease, and 50,000 people die because of heart disease. The report also depicts that over 150,000 people await a kidney transplant every year out of which only 5,000 get among them.
– The Ministry of Health & Family Welfare launched the 6th World and 1st Indian Organ Donation Day and Organ Donation Congress 2010 in New Delhi. It urges people from all communities to donate organs and help the noble cause of saving lives.
You may refer to our last blog regarding the types of organ donations, its process and who all can be donors. In this blog, we will discuss the various organs which can be donated and the laws governing organ donation in India.
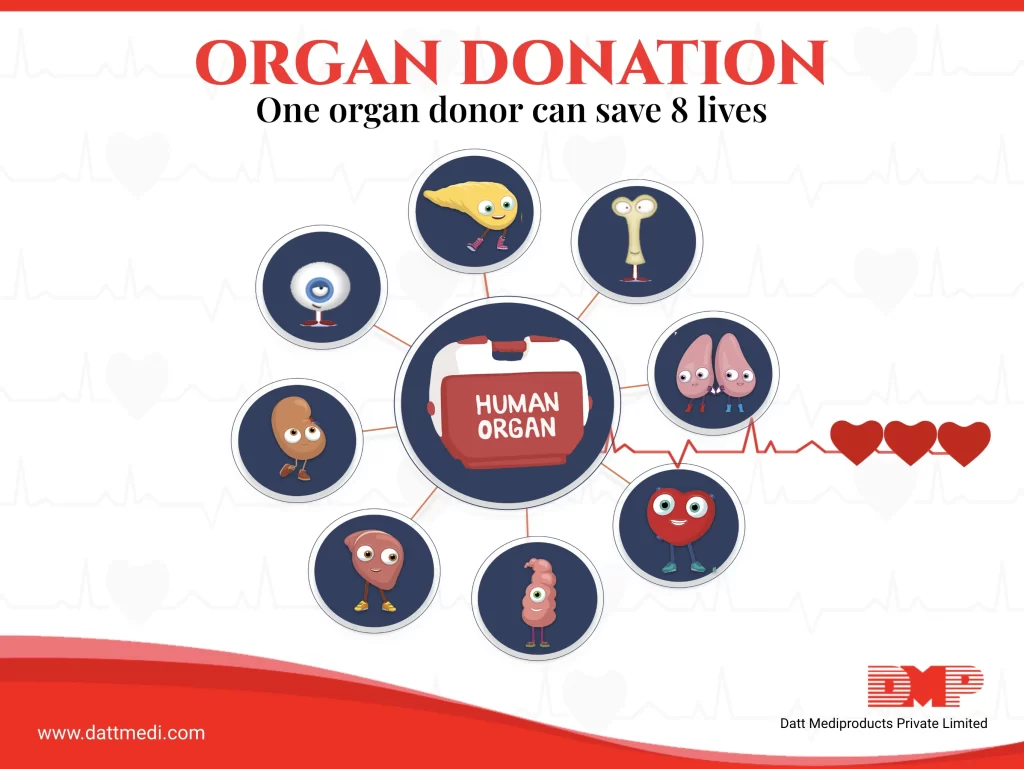
There are 8 main internal organs which can be donated and transplanted into the recipient (apart from the tissues), which are listed below:
1. Kidneys: Kidneys are the most frequently donated organs and an average lifespan of a donated kidney is around 9 years. If the donor is a deceased person, then both kidneys can be donated. On the other hand, a living donor can donate one kidney and function regularly for the rest of the life.
2. Heart: Heart is another important organ which pumps the blood to the entire body. After being recovered from a donor, a heart can live for about 4-6 hours (in proper transportation condition) before being put into a recipient.
3. Liver: Liver is an important function that performs a lot of essential functions like bile production, excretion of bilirubin, cholesterol, hormones; fat metabolism, proteins & carbohydrates metabolism; activation of enzymes; plasma protein synthesis; glycogen storage; blood detoxification & purification. A liver from a deceased donor can be split into 2 parts and transplanted into 2 different recipients. On the other hand, a living donor can donate a part of his/her liver and the rest will regenerate itself to the fullest.
4. Pancreas & Intestines: Both living and deceased donors can donate a pancreas and or intestines. A deceased donor can donate the full pancreas and intestine, while a living donor can donate only a part of it.
5. Lungs: Although lungs can’t regenerate, still living donors can donate a single lobe of their lungs.
6. Skin: Skin can be used for grafting purposes in burn victims, or acid attack victims, etc.
7. Bones: Bones can be retrieved from deceased donors and transplanted in a recipient with the cancerous part.
8. Cornea: Cornea is the most common donated tissue. But, DGHS reports about 25000 corneal transplants performed every year against a requirement of 1 lakh. The cornea is the primary focusing element and people with corneal blindness can be treated with such transplants.
The legal framework in India
The main law which governs the legislation of organ donation and transplantation in India is the “Transplantation of Human Organs Act” (THOA). This act was passed in 1994 and initiated at the request of few states. Later on, it was adopted by other states also excluding AP and J&K.
The main aim of this act is to regulate the retrieval, storage, and transplantation of the organs for therapeutic purposes. This is also to avoid any unethical commercial dealings.
We, Datt Mediproducts intend to raise awareness regarding the shortage of organs availability for transplants, in India. We urge everybody potential to donate organs and to find out about organ donations practices and donor cards in their city. Help save lifes. We also stand against unethical practices and organ trafficking.