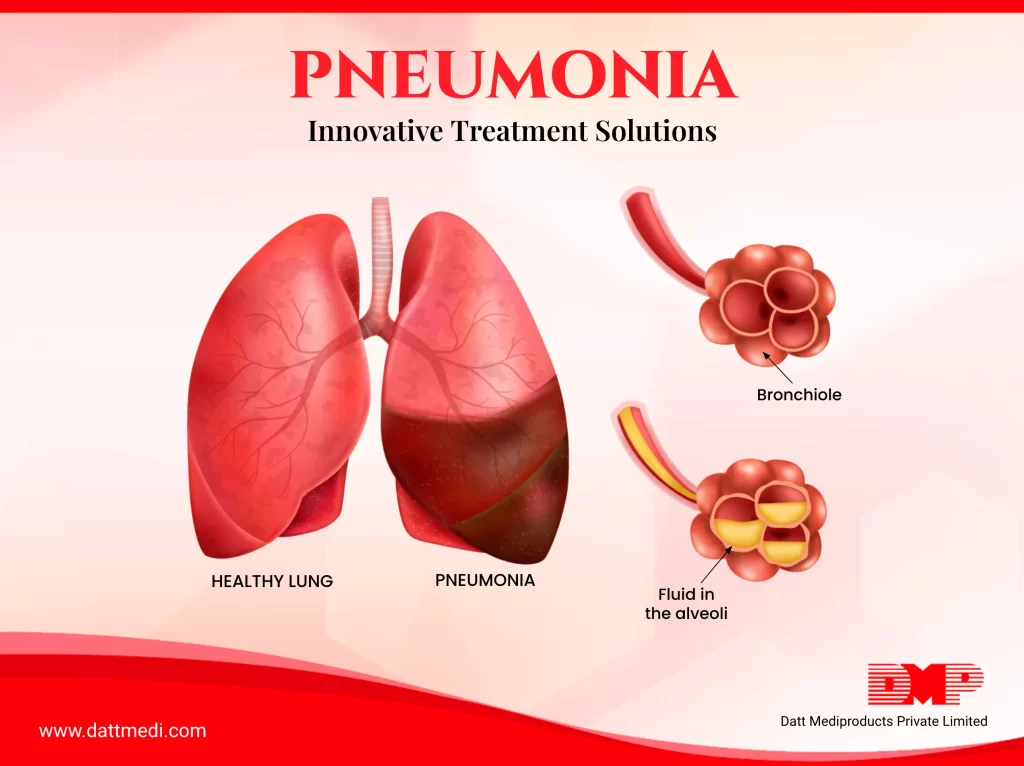
Do you know that Pneumonia is the foremost infectious disease causing death in children below 5 years of age? Let us understand what it is.
Pneumonia is an infection that affects human lungs and causes inflammation of the air sacs. The alveoli (air sacs) might get filled with pus or fluid resulting in cough.
Pneumonia may be caused by bacteria, viruses or fungi, hence its various types.
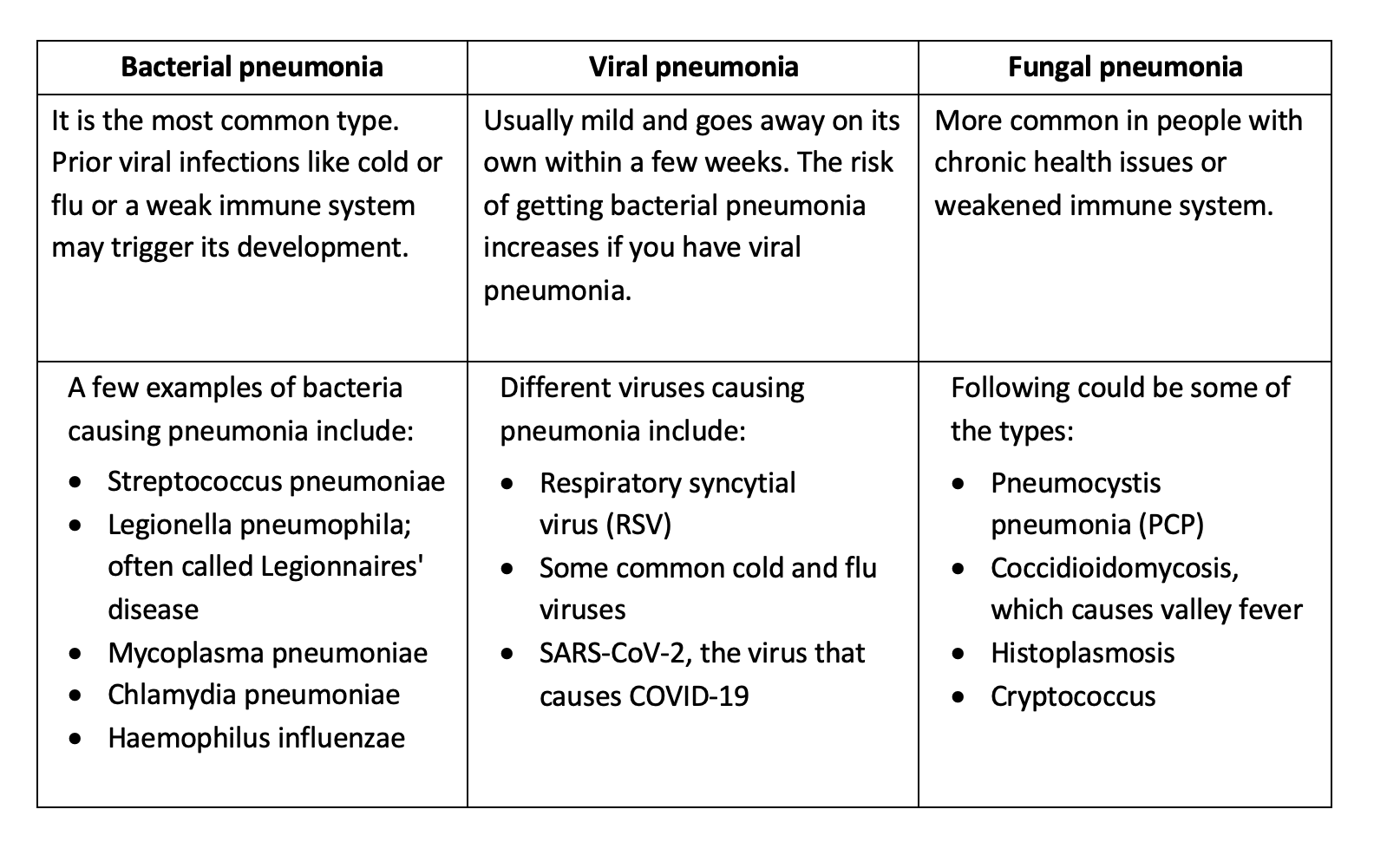
Apart from these, pneumonia may be classified as Hospital Acquired Pneumonia, Healthcare Acquired Pneumonia or Aspiration Pneumonia.
SYMPTOMS
The seriousness of this indication may range from mild to life threatening, depending upon some factors like infection causing agent, age and overall health of the patient. The pus or the purulent material which accumulates in the air sacs causes cough with phlegm or pus, fever, sweating or shaking chills, and difficulty in breathing. Some other signs and symptoms may include the following:
-Chest pain while breathing or coughing
-Confusion or changes in mental awareness (in adults age 65 and older)
-Fatigue
-Lower than normal body temperature especially in adults age 65 or more and people with weak immune systems
-Nausea, vomiting or diarrhea
-Shortness of breath
CERTAIN KEY FACTS
-Pneumonia can occur in one or both the lungs
-As per WHO, Pneumonia accounted for 14% of all deaths of children under 5 years old, killing 740 180 children in 2019
-Only one third of children with pneumonia receive the antibiotics they need
-In spite of various appropriate antibiotic treatments, 14–35% of all hospitalised community-acquired pneumonia (CAP) patients die, which may be due to their age and comorbidities
INNOVATIVE TREATMENT SOLUTIONS
A few innovations to treat childhood pneumonia are under development. These include amoxicillin dispersible tablets, Low-cost, electricity-free oxygen concentrators, oxygen-in-a-box, which relies on chemical oxygen generation.
In 2019, USFDA approved a new antibiotic Xenleta (lefamulin) to treat community-acquired bacterial pneumonia in adults. The safety and efficacy of this drug was evaluated in 2 clinical trials with a total enrollment of 1,289 patients. The clinical success rates were found to be similar when compared to another antibiotic, moxifloxacin with or without linezolid.
ADJUVANT THERAPIES FOR IMPROVING PULMONARY BARRIER FUNCTION
Adrenomedullin: It is an endogenous peptide expressed by different vascular system cells. It improves pulmonary barrier dysfunction caused by different stimuli such as hydrogen peroxide, or Staphylococcus aureusα-toxin. Various studies show Adrenomedullin as a promising candidate for an adjuvant pharmacological approach to prevent lung injury in pneumonia.
Angiopoietin/Tie2 system: Angiopoietin (Ang)-1 and Ang-2 are ligands for the receptor tyrosine kinase Tie2. A short synthetic peptide VASCULOTIDE inhibits binding of these ligands and has proven to have therapeutic potential by counteracting lung vascular barrier dysfunction and reducing mortality.
Apart from these, stem based therapies are also available for pneumonia associated acute respiratory distress syndrome (ARDS).
We understand that it might take time to recover from pneumonia but trying to treat the indication on your own without consulting a doctor might not be a good option to consider.
Avoid taking cough medicines also, as cough is one of the body’s responses to get rid of infection. We @dattmediproducts recommend consulting a doctor at every step. The only precaution one can take is to stay away from smoke to help your lungs heal and take a lot of rest.