Both malaria and dengue are mosquito-borne diseases and are a cause of high mortality and morbidity in many countries mainly tropical. Both these conditions have an ability to cause acute febrile illness (an illness related to fever), but still, they are fundamentally different.
We bring some facts to help understand them better. Before discussing the differences here are some facts about the diseases from the World Health Organization (WHO).
People living in the poorest countries are at a higher risk of malaria, which is approx. 40% of the world’s population
– Every year, malaria affects more than 200 million people worldwide.
– Every 2 minutes, a child dies of malaria.
– WHO estimates around 390 million cases of dengue infection worldwide every year, out of which 96 million manifests clinically.
– WHO launched the Global Malaria Programme (GMP) to help prevent, control and study malaria.
Following are the various characteristic differences between these two fatal monsoon diseases:
- DISEASE AGENT: Malaria is a protozoal infectious disease while Dengue is a viral infection. Both are mosquito-borne diseases but the main mosquito vector of malaria is Anopheles while for dengue its Aedes.
- MODE OF TRANSMISSION: Malaria is transmitted through the bite of the female Anopheles mosquito carrying Plasmodium parasite. While Dengue is spread by the female mosquito biting an infected person and then transmitting the virus by biting a healthy person, usually in the early morning or at dusk.
- ILLNESS TYPE: The incubation period, in the case of malaria, may last for 7-30 days, before the first symptom appears. In some cases, the disease can relapse months or years later without any visible symptoms. In the case of Dengue, symptoms begin 4-7 days after the mosquito bite and last for 5-10 days. Symptoms vary depending on the severity of the disease.
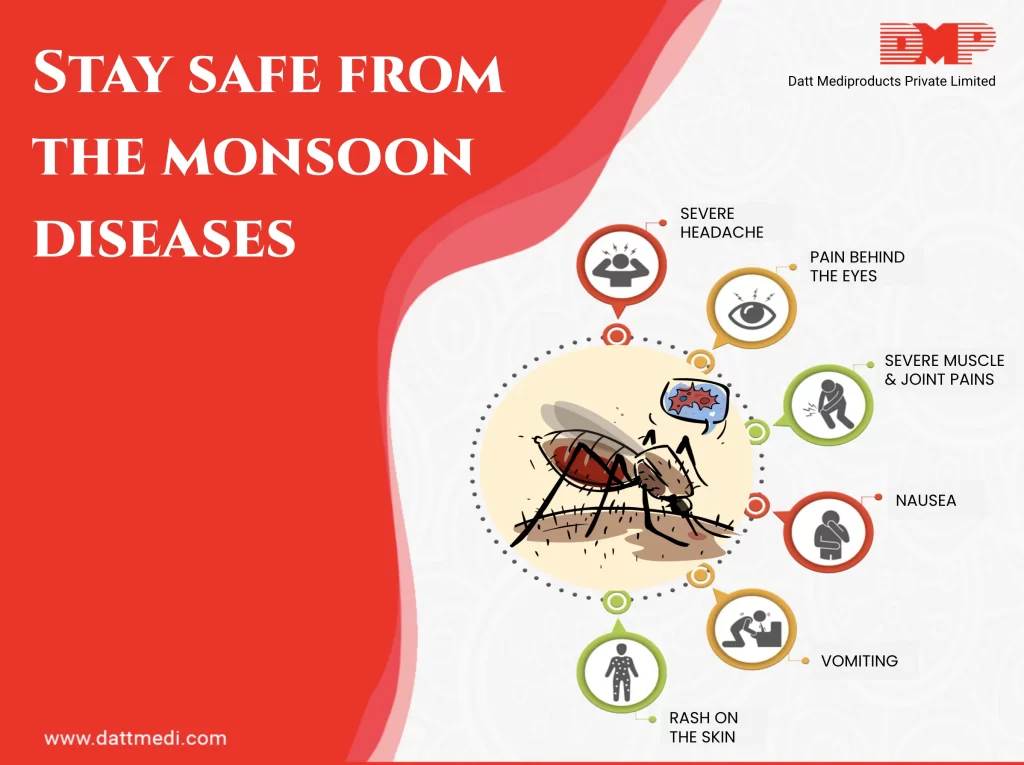
- SYMPTOMS: Malaria may exhibit symptoms like fever, chills, headache, nausea, vomiting, muscle pain and fatigue. Patients with Dengue may show symptoms like pain behind the eyes, swollen glands, and rashes apart from some common symptoms like high fever, fatigue, nausea, and vomiting.
- BLEEDING: The chances of bleeding in Malarial infection is rare while Dengue can result in internal bleeding caused by any capillary burst.
- HEMOLYSIS: The malarial parasite infects human liver cells, increasing their number and causing the liver cells to rupture. The sporozoites of the parasite then invade the RBCs constantly altering their structure and causing them to rupture. The toxic substances collected in the infected cells get released and the infection spreads to other cells and the cycle continues.
- THROMBOCYTOPENIA: Dengue virus can damage the bone marrow and result in a drop of white blood cells and platelet count from normal range (1.5-4 lacs) to as low as 20,000. Chances of thrombocytopenia in malarial infection are rare.
COMPLICATIONS:
– Malaria: can be a fatal disease-causing one or more serious complications like cerebral malaria, breathing problems, organ failure (liver, kidneys, spleen rupture), anemia and low blood sugar to name a few.-Dengue: A severe form of Dengue fever, also called “Dengue Hemorrhagic fever”, can damage the lungs, liver or heart. Resulting in severe bleeding and a sudden drop in blood pressure to dangerous levels causing shock and death.
TREATMENT: Malaria & Dengue both are potentially fatal diseases and treatment should be initiated as soon as possible.
-Dengue: Also known as break-bone fever can’t be cured. Unfortunately, there is no vaccine for dengue fever and no specific treatment; the condition can only be controlled with a combination of drugs and intravenous infusion. Blood and platelet transfusion may be required in case of a major loss.High fever & vomiting can dehydrate your body. Rehydration salts can help replace the lost minerals and fluids in the body. Pain killers such as paracetamol can help lower fever and ease the pain. NSAIDs are nor advised in dengue patients as they might increase the risk of internal bleeding.-Malaria: The treatment option for severe malaria cases include continuous intravenous infusion for those who can’t take oral medications. The drugs used to treat the active parasitic forms in the blood include Chloroquine, Mefloquine, Quinine and Doxycycline/ Clindamycin/ Tetracycline in combination with quinine. Drugs like primaquine and tafenoquine are also available which are active against the dormant parasitic liver forms) and help prevent relapses.
Although both the diseases differ in various characteristics, the risk factors like unhygienic neighborhoods, tropical weather, and exposure to the virus are the same.We @DattMediproducts Pvt. Ltd. recommend everybody to not allow the water to stagnate in neighborhoods, using mosquito repellents while in outdoors, keep food covered at all times, and staying clean and washed in this monsoon season to prevent and lower the risk of lowering these dangerous diseases.