Allergies are a common health issue that affect a significant portion of the population worldwide. Allergies are a hypersensitive reaction of the immune system to an otherwise harmless substance, which is known as an allergen. The allergen can be any substance that triggers an allergic reaction in the body, such as pollen, dust, food, or animal dander.
Allergies are caused due to the abnormal response of the immune system, which mistakes a harmless substance for a harmful invader and initiates a defence mechanism, called antibodies, to protect the body from it. This results in various allergic reactions, such as skin rashes, itching, sneezing, watery eyes, and in severe cases, anaphylaxis.
There are various reasons behind the occurrence of allergies. Genetics plays a significant role in determining an individual’s likelihood of developing allergies. Environmental factors such as exposure to pollution, chemicals, and toxins can also trigger allergies.
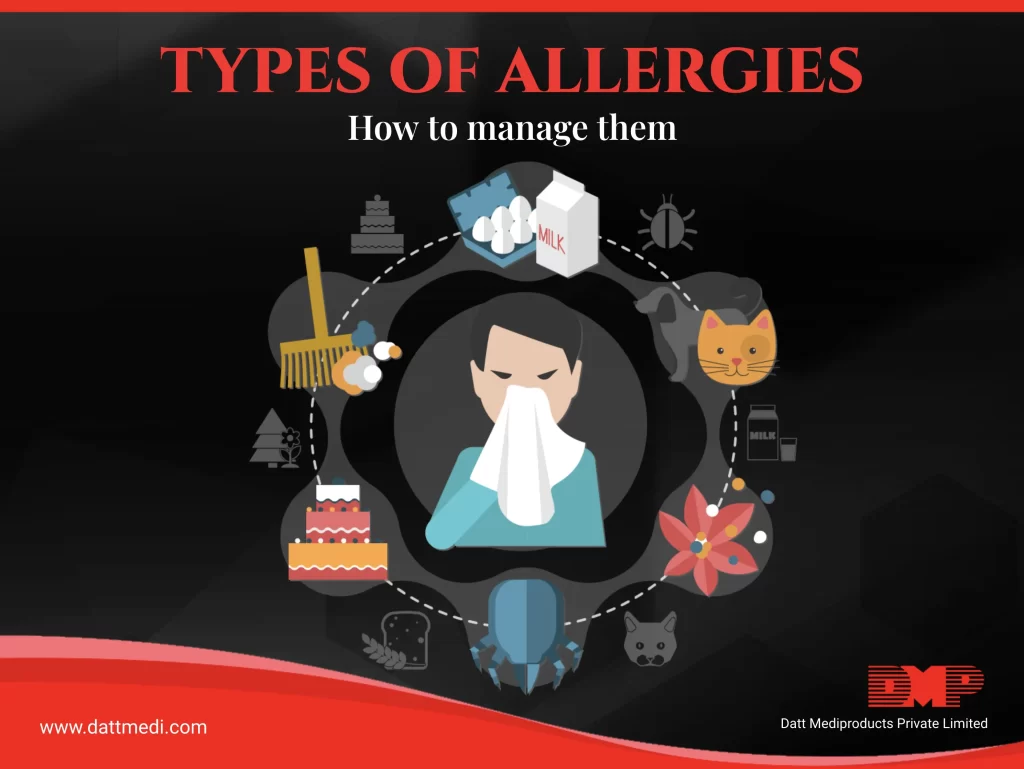
There are several different types of allergies, each with their unique symptoms and triggers.
Some of the most common types of allergies include:
1. Respiratory allergies:
These allergies are triggered by airborne allergens such as pollen, dust mites, and animal dander. The symptoms of respiratory allergies include sneezing, coughing, and wheezing.
2. Food allergies:
These allergies occur when the immune system reacts to certain foods, such as nuts, shellfish, and eggs. Symptoms of food allergies can range from mild itching, tingling in the mouth, hives, swelling of the lips, tongue, face or throat to more severe life-threatening anaphylaxis.
3. Skin allergies:
These allergies occur when the skin comes into contact with an allergen, such as certain fabrics, metals, or cosmetics. The symptoms of skin allergies include rashes, itching, and swelling.
4. Insect allergies:
These allergies occur when an individual is bitten or stung by an insect, such as bees or mosquitoes. The symptoms of insect allergies can range from mild itching to severe anaphylaxis.
5. Medicine allergies:
Medicine allergies are hypersensitive reactions of the immune system to certain medications. They can cause symptoms like skin rashes, itching, swelling, and in severe cases, difficulty breathing or anaphylaxis. It is important to communicate medicine allergies to healthcare providers to ensure safe and effective treatment.
Precautionary methods can be taken to manage allergies. Firstly, it is crucial to identify the allergen that triggers the allergic reaction. This can be done through various tests such as skin tests or blood tests. Once the allergen is identified, it is essential to avoid exposure to it. For example, individuals with food allergies must avoid eating the allergen-containing food.
Similarly, those with respiratory allergies must avoid exposure to airborne allergens, such as pollen or animal dander. If a person has a known severe allergy then they can also wear a medical alert bracelet, which lets others know that you have a serious allergy incase they are unable to communicate it.
Medications such as antihistamines, decongestants, and corticosteroids can be used to manage allergy symptoms. In severe cases, epinephrine injections may be required to manage anaphylaxis.
In addition to medication, several lifestyle changes can also help manage allergies. One of the most important being to try to reduce stress levels. While stress can’t trigger an allergic reaction it can make it worse if you are having one. When in stress your body releases hormones including histamine, which is a powerful chemical that leads to allergy symptoms thus making the reaction worse.
Allergies can significantly impact the lives of those who suffer from them. However, with proper management, it is possible to reduce the severity of allergy symptoms. If you suspect that you have an allergy, it is important to seek medical advice and get a proper diagnosis.
We advice to follow precautionary methods and working with a healthcare professional, that can help you manage allergies and improve your quality of life. Follow us for more such information.