HIV is a virus that causes damage to the immune system by destroying the white blood cells in the body. First identified in the year 1981, Human Immunodeficiency Virus (HIV) interferes with the body’s ability to fight against disease-causing microorganisms. It destroys CD4 cells (a type of T-helper cells that move around the body & detect anomalies & infections), makes copies of itself and weakens an individual’s immune system.
When CD4 counts drop below 200 it is an indication of serious immune damage and a person is diagnosed with AIDS. The normal range for CD4 cells is about 500-1500.
How HIV becomes AIDS?
AIDS stands for Acquired Immune Deficiency Syndrome and is the most advanced stage of HIV infection. AIDS is the set of symptoms caused by infection from a virus, known as HIV.
HIV contraction leads to AIDS but it doesn’t mean that all individuals with HIV infection will develop AIDS. HIV progression varies from individual to individual. Although there is no cure for HIV, medications may help to slow its progression.
STAGE 1: ACUTE PHASE: Primary Infection
This phase generally lasts for a few weeks and people infected may develop flu-like symptoms such as fever, headaches, joint pain, muscle pain, rashes, swollen lymph glands, sore throat, etc. Symptoms are so mild that they are unnoticeable. But the viral load increases in the acute phase itself and very easily spread to the next phase.
STAGE 2: CHRONIC HIV: Clinical Latency (HIV inactivity or dormancy)
During this stage, HIV continues to multiply in the body but at very low levels. People in this stage may not even get any of the HIV-related symptoms. This stage may last for 10 years if the patient is not on antiretroviral therapy. In some people, the infection may advance much sooner. However, people who take HIV (ART) medicine as prescribed may be in this stage for several decades.
STAGE 3: Symptomatic HIV Infection: AIDS
Thanks to the available ART treatments, the chances of developing AIDS have decreased drastically. AIDS is the most severe stage of the infection and occurs when the immune system is severely damaged. The risk of developing opportunistic infections or cancers also increases as a result.
Do You Know?
World AIDS Day was observed on 1st December 1988 for the first time with the theme “Join the Worldwide Effort”. This date was designated by WHO and supported by the United Nations.
How HIV do and doesn’t Transmit?
HIV is a sexually transmitted infection (STI). It transmits through body fluids including infected blood, semen, vaginal & rectal fluids and from mother to child during pregnancy, birth or even breastfeeding.
Do you know that “UNDETECTABLE=UNTRANSMITTABLE”? If HIV can’t be detected, it means it can’t be transmitted to others, even after the transfer of body fluids because of the very low count of HIV virus. If you are treated for HIV early in your pregnancy, the risk of transmitting HIV to your baby can be 1% or less.
HIV doesn’t transmit through air or water, or through casual contact. It can’t spread through sweat, saliva or urine.
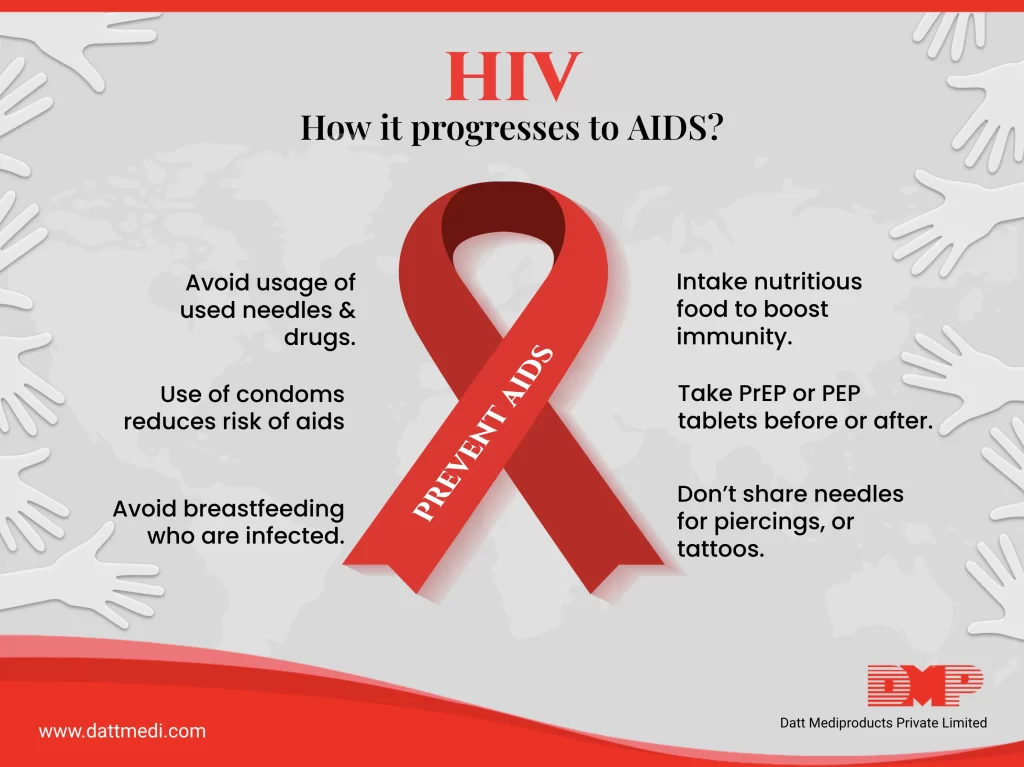
PREVENTING HIV:
There is no vaccine to prevent HIV transmission but the risk of contracting the infection can be lowered by taking certain steps:
– Avoid sharing needles and syringes as they may be contaminated with HIV or even the Hepatitis virus.
– Have safer sex by using protection, getting tested for HIV & other sexually transmitted infections on a regular basis.
– Mothers should not breastfeed their children if they are HIV positive, breast milk can carry the HIV virus.
– Contact a medical healthcare provider to talk about taking PrEP (pre-exposure prophylaxis) and PEP (post-exposure prophylaxis) before and after being exposed to the HIV virus. This reduces the risk of contracting the virus.
– Take the ART medications as directed by the physician.
We @ Datt Mediproducts understand that there is no cure of HIV, but with treatment it can be controlled and the progression can slow down. We recommend getting tested for HIV regularly so that you can get the antiretroviral treatment when you need it. If people with HIV take ART as prescribed, their viral load can become undetectable. By following the preventive measures, one can live a healthy and long life.




