As we age, our bodies undergo various changes, and one aspect that demands special attention is wound healing. Seniors, due to their aging skin, often face challenges in this regard.
In this blog post, we’ll delve into the unique needs of wound care for seniors at home, providing insights and recommendations for a more effective and comfortable healing process.
Understanding Age-Related Wound Healing
The aging process affects the skin’s ability to heal. Seniors may experience a slower healing process due to factors like reduced collagen production and thinner skin. It’s crucial to comprehend these changes to implement targeted wound care.
Mobility and Accessibility Considerations
Seniors might encounter difficulties in accessing wound care supplies. To address this, consider creating a designated and easily accessible area for supplies. This minimizes the challenges related to mobility, ensuring that seniors can conveniently reach essential items for dressing changes.
Sensitive Skin and Wound Care Products
Seniors often have sensitive skin that requires special attention. Opt for hypoallergenic and non-irritating wound care products. This choice not only promotes healing but also prevents additional discomfort for seniors with delicate skin.
Regular Monitoring and Assistance
Regular monitoring of wounds is crucial. Encourage caregivers or family members to play an active role in this process. Timely detection of any changes can help prevent complications and ensure a smooth healing journey for seniors.
Pain Management and Comfort
Managing pain effectively is paramount for seniors. Recommend suitable pain relief methods and medications appropriate for their age group. Ensuring comfort during the healing process contributes significantly to overall well-being.
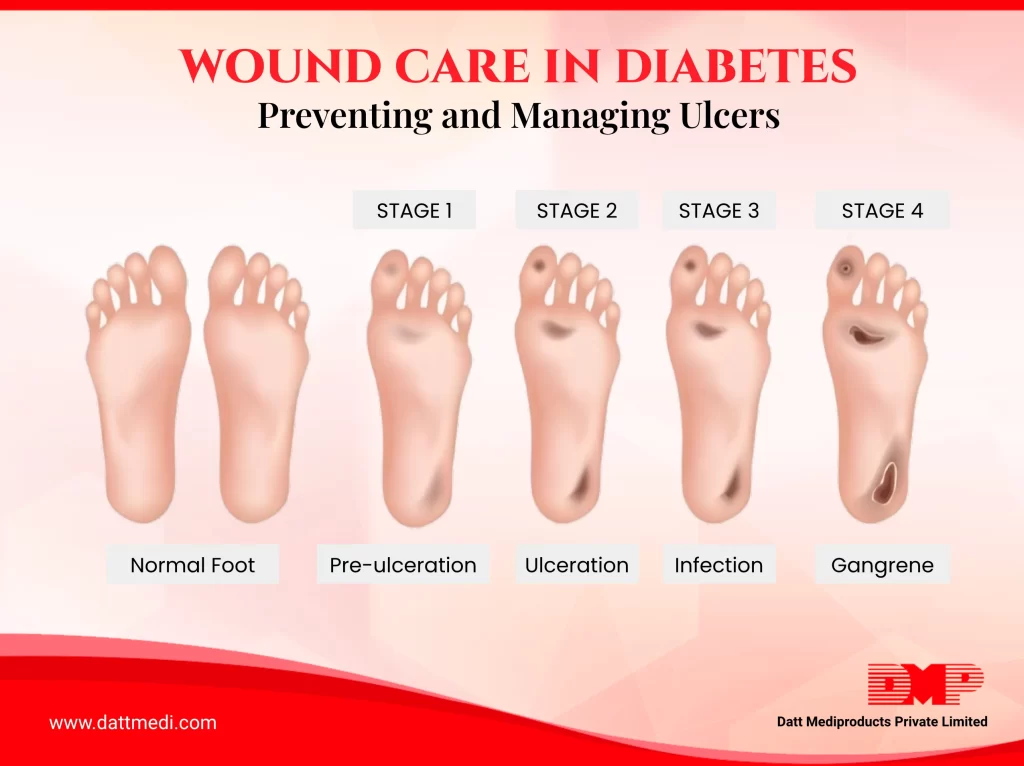
Preventing Complications and Infections
Prevention is key to avoiding complications, especially infections. Educate seniors on the signs of infection and stress the importance of seeking immediate medical attention if any concerns arise. A proactive approach significantly reduces the risk of complications.
Communication with Healthcare Providers
Encourage open communication between seniors and their healthcare providers. Stress the importance of reporting any changes or concerns promptly. A collaborative effort between seniors, caregivers, and healthcare professionals ensures a comprehensive and personalized approach to wound care.
Therefore, addressing the unique needs of wound care for seniors at home involves a multifaceted approach. Understanding age-related changes, considering mobility challenges, using gentle products, regular monitoring, effective pain management, preventive measures, and open communication are key elements in promoting optimal healing for seniors.