Wound Healing is a complex and dynamic process. It involves 3 to 4 distinctive phases in order to replace devitalised and missing cellular structures and tissue layers.
Wound healing is a normal biological process of human body.
But, healing gets delayed when wounds become infected with harmful microorganisms. If left untreated, there is also a risk of the infection spreading to other body parts.
Negative Pressure Wound Therapy (NPWT) is an effective procedure for the treatment of wounds of various aetiologies and is not less than any gold standard technique for the management of complex non-healing wounds.
It involves applying a continued sub-atmospheric pressure at wound bed site, to increase blood flow to the area and withdraw excess fluid from the wound to promote wound healing.
NPWT system consists of a dressing and a vacuum source. The various components of dressing include an open pore foam, a transparent adhesive dressing, a tubing to connect the dressing with a vacuum pump producing negative pressure and a canister to collect the exudates. The technique is used an adjunct to surgical debridement to treat tissue defects around open fractures and chronic, contaminated wounds.
Do You Know? “The advent of modern NPWT systems is attributed to Argentas and Morykwas, who developed several prototypes to facilitate wound healing by distributing suction across wounds to help draw the skin edges together- Annals of Plastic Surgery”.
Mechanism of Action:
NPWT facilitates wound healing at both macroscopic & microscopic levels.
– The primary mechanism of action includes wound edges contraction called “tissue macro-deformation” powered by the suction, distributed through the dressing foam.
– Secondly, NPWT results in “micro-deformation” by promoting cell division and proliferation, growth factor production and angiogenesis.
-Next important step includes the removal of oedematous fluid and exudates from the extracellular space, thereby removing inflammatory chemicals and cytokines.
– A warm and moist environment wards off wound desiccation and enhances the formation of granulation tissue.
Clinical Indications:
NPWT therapy has been studied across all medical and surgical specialties and as of Jan.2014, the technique has been mentioned in over 861 peer-reviewed journals. Its potential has been demonstrated in various contaminated, difficult to treat wounds covering both acute and chronic types.
There have been increasing evidences on NPWT’s ability to aid the closure of various acute wounds such as Traumatic & Surgical Wounds and Subacute & dehisced wounds. NPWT technique is found to be valuable in management of various chronic wounds such as Pressure Ulcers, Diabetic Foot Ulcers (DFU), Arterial and Venous Leg Ulcers. Applying NPWT to a newly laid down skin graft is gaining importance with a number of studies showing an improvement in graft incorporation by using a pressure ranging between -50 to -80 mmHg.
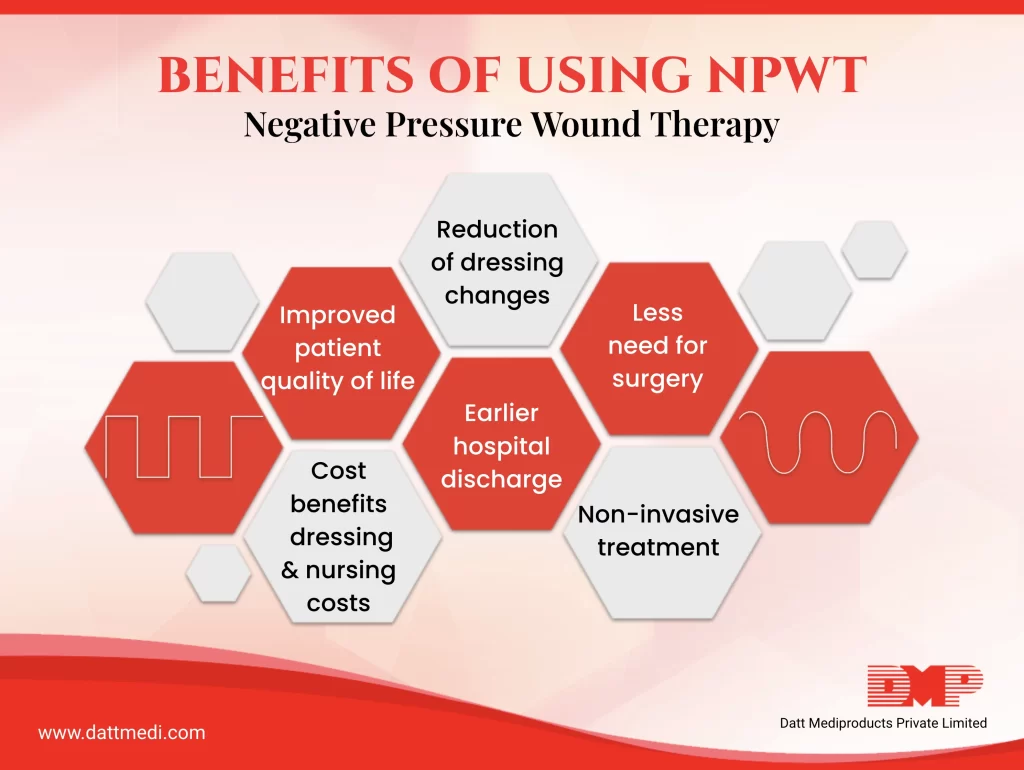
The benefits of using NPWT over conventional dressings have been documented.
– The therapy offers a non-invasive treatment with one of the major advantage being reduction in number of dressing changes, which in turn improves compliance as the patient suffers less pain and inconvenience when compared with conventional dressings.
– The negative pressure removes excess fluid allowing for enhanced circulation and disposal of cellular waste, thereby reducing the risk of bacterial contamination.
-NPWT eases the formation of a local infection-free healing tissue in a short period of time. Thereby, preventing the need for complex surgical procedures for the final coverage of important structures.
-A faster reduction in the wound size and formation of granulation tissue with rapid wound closure has been observed as compared to conventional dressings.
-The speedy wound management with NPWT enables transfer from hospital to lower-cost health care setting. Apart from these its saving on the dressing & nursing costs too.
We are a leading manufacturers and marketers of NPWT devices and consumables in India. Our product with brand name “VEL NeXT” is CE certified being audited by SGS Belgium NV, Notified Body 1639. VEL NeXT is approved and licensed by “Central Drugs Standard Control Organization (CDSCO), Ministry of Health, Government of India.
The various consumables are produced and packed in a controlled environment following stringent quality measures.
Visit our website www.dattmedi.com to know more.




