Have you ever felt pain, swelling, and stiffness in your joints or trouble moving around? You might be suffering from a condition called “Arthritis”.
Arthritis is defined as the inflammation or swelling in one or more joints.
The two most common types are Osteoarthritis and Rheumatoid Arthritis. Symptoms vary from person to person but the main ones include joint pain and stiffness. Arthritis treatment may depend on its type but the goal of treatment is to reduce symptoms and improve the quality of life of the affected person.
Early Signs:
There may be several symptoms depending upon the type but the usual ones are joint pain and stiffness. Symptoms may come and vanish and may range from mild to moderate to severe ones. Common symptoms include:
- Swelling
- Pain
- Redness
- Stiffness
- Decreased range of motion
It is possible that symptoms remain unchanged over years but they progress over a period of time. People affected with severe conditions may feel chronic pain. The condition may make them unable to do their daily activities and even difficult to walk.
The Different Types
OSTEOARTHRITIS:
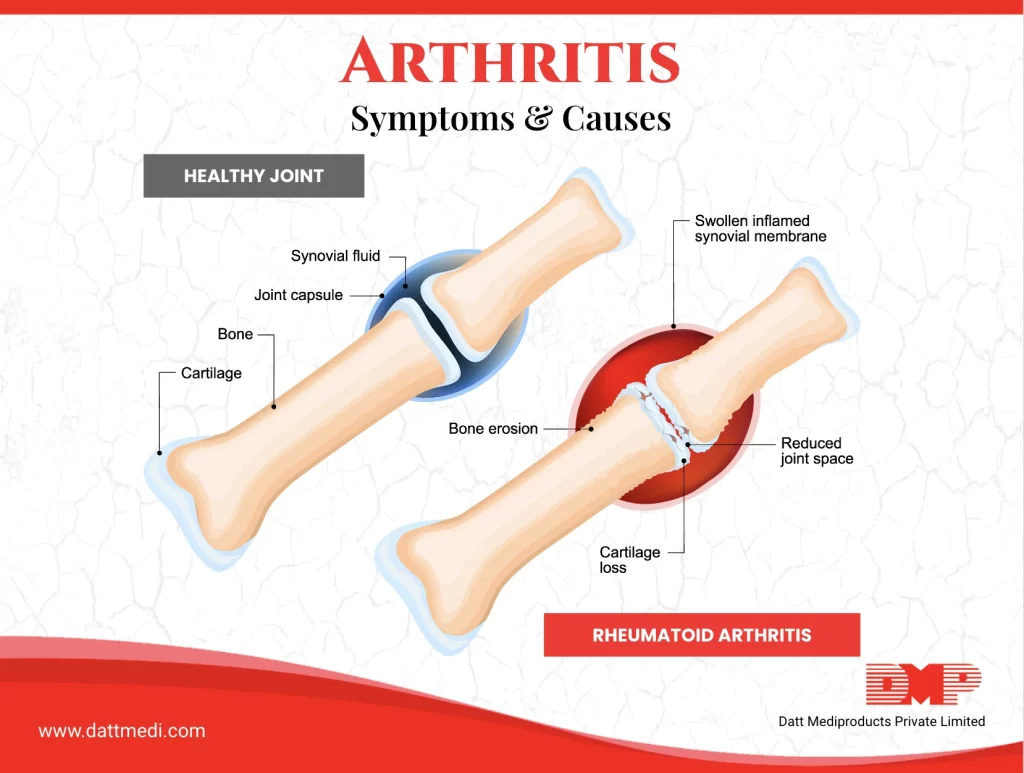
It is the most common type of arthritis. Osteoarthritis occurs when the protective cartilage, present between two bones, wears down over time. Osteoarthritis can affect joints of your hands, knees, hips, and spine.
RHEUMATOID ARTHRITIS:
RA is an autoimmune condition that occurs when the body’s immune system attacks the linings of your joints healthy cells of the body by mistake. This causes inflammation of synovial layer, releasing chemicals to damage the nearby bones. Rheumatoid arthritis usually attacks multiple joints at once. The affected joints are generally the ones in the hands, wrists, and knees. In RA, joint lining becomes inflamed, thereby damaging the joint tissue. The inflamed joint lining and damaged joint tissues result in chronic pain, unsteadiness, and deformity.
JUVENILE IDIOPATHIC ARTHRITIS:
It is the most common type of arthritis affecting children under 16 years of age. Formally known as “Juvenile Rheumatoid Arthritis”, it can cause a persistent joint pain, stiffness, and swelling. It may also lead to some serious complications such as joint damage, eye inflammation, and problems with the growth of the child.
SEPTIC ARTHRITIS:
Septic or Infectious arthritis is a painful infection that has spread from another part of the body to the joint. The infection can come from germs traveling through the bloodstream or through a penetrating injury delivering germs directly into the joints.
PSORIATIC ARTHRITIS:
This is a form of arthritis that affects people with psoriasis (a skin condition featuring red patches topped with silvery scales. It can affect any body part including the spine and fingertips. There is no cure for Psoriatic Arthritis but the symptoms can be managed to prevent damage to the joints.
GOUT:
Gout is a painful and complex type of arthritis. It develops when too much uric acid builds up in the body. Symptoms include sudden and severe pain attacks with swelling, redness, and tenderness in the joints. It often starts at the base of the big toe. The joint becomes so tender that even a feather-like weight may seem intolerable.
The symptoms may vary with the type of arthritis you are suffering from, but pain and stiffness are the most common ones. We @dattmediproducts recommend practicing some strategies and activities to reduce arthritis symptoms and get relief.
These activities may include being physically active, which reduces stress, improves function & quality of life; consulting a doctor to get an accurate diagnosis and treatment to minimize symptoms, and delay disease progression.
Above all, try to maintain a healthy weight which particularly helps to reduce stress on joints and improve pain and function to lead a better and managed life for people with arthritis.