In developing nations, acute diarrheal diseases and dehydration caused by them are one of the most significant causes of death in infants and young children. This dehydration can be managed orally and intravenously, with oral rehydration therapy being the most effective, simple to use, and worthwhile of the two options.
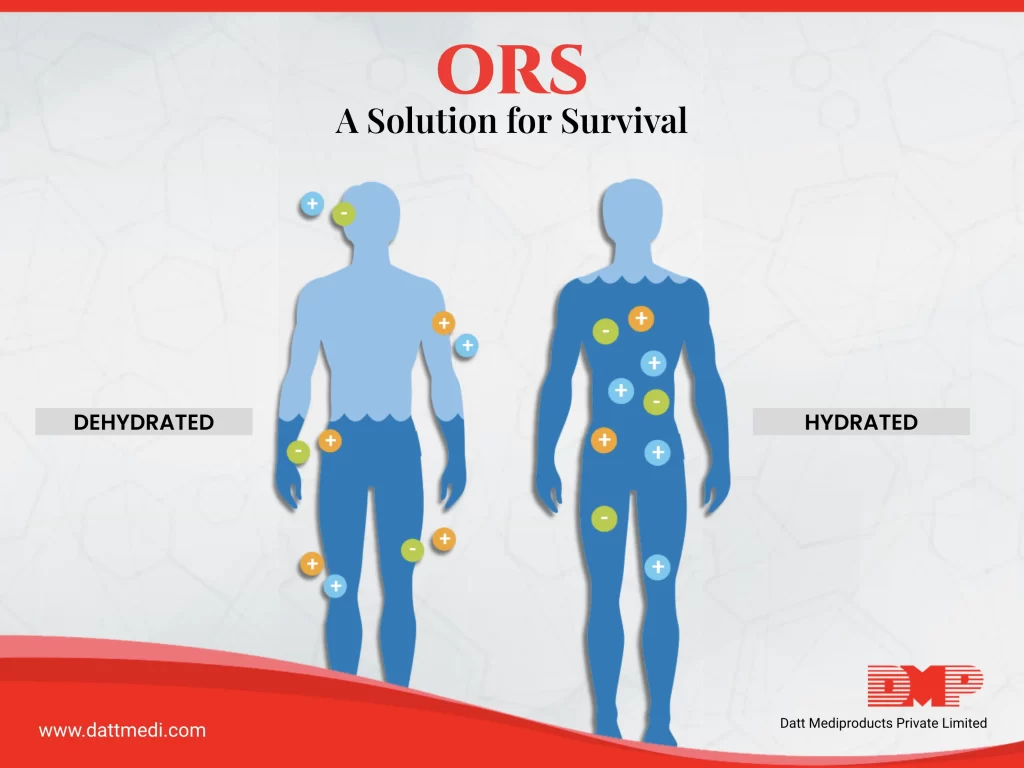
Definition: Dehydration is defined as the loss of water and dissolved salts from the body, occurring, for instance, as a result of diarrhoea and the correction of dehydration is called as Rehydration.
Oral Rehydration Therapy: The Solution is in Your Hands
WHO defines Oral Rehydration Therapy (ORT) as “The administration of fluid by mouth to prevent or correct the dehydration that is a consequence of diarrhoea”. This fluid consists of a special mixture of water, glucose and salts which help to replenish the lost electrolytes and water and bring it back to normal levels. ORT is an effective treatment method to manage dehydration and a powerful alternative to intravenous therapy.
The WHO Department of Child and Adolescent Health and Development (CAH) in collaboration with UNICEF recommend Oral Rehydration Therapy (ORT) as the main strategy to achieve a reduction in diarrhoea-related mortality and malnutrition in children.
ORS Composition
Oral Rehydration Salts (ORS) is the non-proprietary name for a balanced glucose-electrolyte mixture. ORS was approved, recommended and distributed by WHO and UNICEF for the first time in 1969 as a treatment option to manage dehydration throughout the world.
Reduced osmolarity solutions have been introduced by WHO and UNICEF, especially for children, to increase the safety and efficacy and subsequently reduce the stool output.
| Reduced osmolarity ORS | grams/litre | Reduced osmolarity ORS | mmol/litre |
| Sodium chloride | 2.6 | Sodium | 75 |
| Glucose, anhydrous | 13.5 | Chloride | 65 |
| Potassium chloride | 1.5 | Glucose, anhydrous | 75 |
| Trisodium citrate, dihydrate | 2.9 | Potassium | 20 |
| Citrate | 10 | ||
| Total Osmolarity | 245 |
If ORS is unavailable, then a mixture of 6 level teaspoons of sugar, 1/2 level teaspoon of salt dissolved in 1 litre of clean water can be given to a child. Extra care must be taken while mixing the components as too much sugar can worsen diarrhoea and too much salt can be dangerous for the child.
How Oral Rehydration Works?
1. In a healthy individual, water is continuously exchanged through the intestine’s walls. Nearly 20 litres of water is secreted and reabsorbed every 24 hours. This physiological process also allows the absorption of soluble metabolites (from the digested food) into our bloodstream.
2. In an individual suffering from diarrhoea, this balance of secretion and resorption gets disturbed, resulting in more secretion than resorption. This causes several litres of water loss in a day along with a significant reduction in sodium levels.
3. Sodium is an essential mineral present in the form of Na+ in blood plasma and body fluids i.e. extracellular fluids. Dehydration causes irregulated sodium levels and rapid depletion of water along with Na+. For proper functioning of the body, about 135-150 mmol/l of Na+ are required to be present in the extracellular fluid.
Do you know?
Depletion in more than 10% of the body fluids might result in acute kidney failure subsequently leading to Death.
4. If we only give saline solution to treat diarrhoea, it may worsen the situation. This is because the mechanism for Na+ absorption by the intestinal wall is impaired in diarrhoeal state and the presence of excess Na+ could further result in water secretion worsening diarrhoea.
5. Adding glucose/dextrose to the saline solution initiates a “co-transport coupling mechanism” as a result of which, each molecule of glucose being absorbed by the intestinal wall helps in the transportation of one molecule of Na+. A relatively increased concentration of sodium inside the intestinal wall pulls water through it, as glucose only co-transports Na+ and not water.
Do you Know?
The co-transport coupling mechanism of Na+ and glucose is reported as “potentially the most important medical advance this century” by THE LANCET journal.
Other molecules with an aptitude to co-transport Na+ through the intestinal wall are amino acids, dipeptides and tripeptides. Oral Rehydration Therapy (ORT) is useful for the treatment of dehydration in patients suffering from prolonged diarrhoea, gastroenteritis, vomiting.
We @ Datt Mediproducts recommend oral rehydration solution as an excellent therapeutic technique for rehydration as “Rehydration Saves More Children”