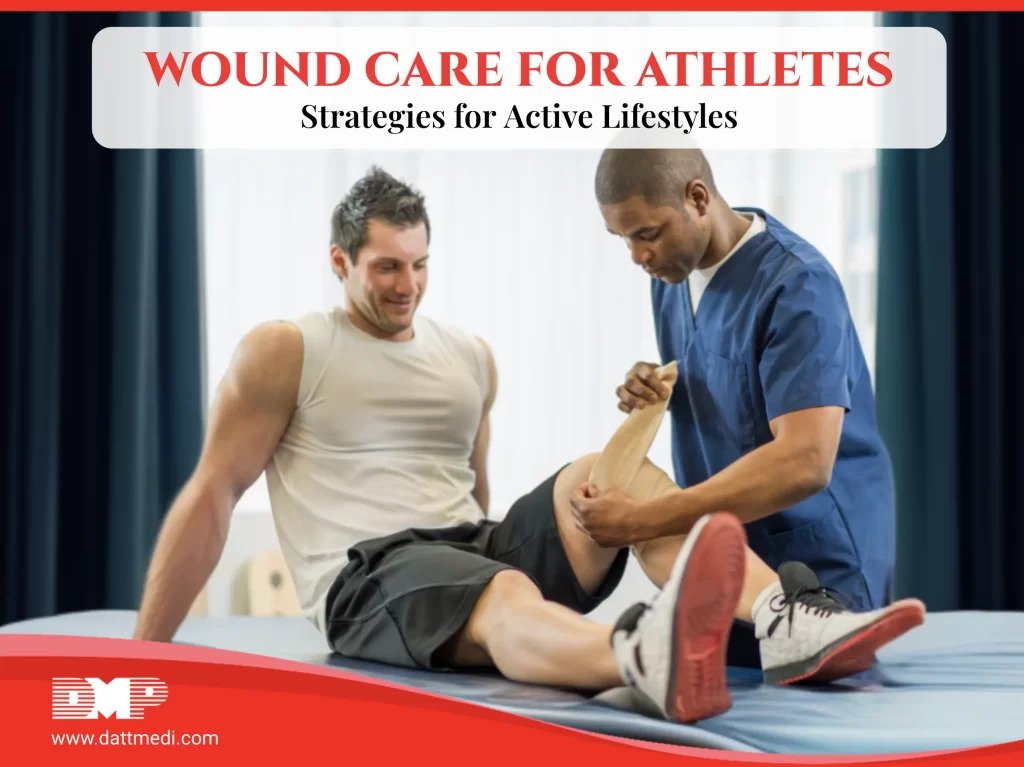
Athletes constantly push their bodies to the limit, making them more prone to injuries and wounds. From minor cuts and bruises to more serious sprains and strains, managing these injuries effectively is crucial for maintaining peak performance and ensuring a swift recovery. This blog delves into effective wound care strategies for athletes and highlights how the innovative Velcool® cooling and compression bandage can play a pivotal role in their recovery.
Understanding Common Athletic Injuries
Athletic activities can lead to a variety of injuries, including:
- Sprains and Strains: Overstretching or tearing of ligaments and muscles.
- Bruises: Caused by impact, leading to bleeding under the skin.
- Cuts and Abrasions: Resulting from falls or contact with rough surfaces.
- Overuse Injuries: Such as tendonitis, caused by repetitive motion.
The RICE Method: A Foundation for Acute Injury Management
The RICE method is a tried-and-true approach for managing acute sports injuries. It stands for Rest, Ice, Compression, and Elevation, each component playing a vital role in minimizing damage and speeding up recovery.
- Rest: Essential to prevent further injury and allow the body to begin the healing process. Avoiding stress on the injured area helps prevent exacerbation of the damage.
- Ice: Applying ice reduces pain and inflammation by constricting blood vessels, limiting blood flow to the affected area.
- Compression: Helps reduce swelling and provides support to the injured tissue by limiting fluid accumulation around the injury.
- Elevation: Keeping the injured part above the level of the heart reduces swelling, associated pain, and discomfort.
Introducing Velcool® : Enhancing the RICE Method
Velcool® is a state-of-the-art cooling and compression bandage that adheres perfectly to the principles of the RICE method. It offers several benefits that make it an indispensable tool for athletes.
Strategies for Effective Wound Care in Athletes
1. Immediate Attention:
- Address injuries immediately to prevent them from worsening.
- Use products like Velcool® for instant cold and compression therapy.
2. Proper Cleansing:
- Clean cuts and abrasions thoroughly to prevent infection.
- Use antiseptic solutions and keep the wound covered with sterile dressings.
3. Monitor Healing:
- Regularly check the injury for signs of infection or complications.
- Adjust the level of activity based on the healing progress.
4. Nutrition and Hydration:
- 4a. Maintain a balanced diet rich in proteins, vitamins, and minerals to support the healing process.
- 4b. Stay hydrated to promote overall health and recovery.
5. Gradual Return to Activity:
- Gradually reintroduce physical activity to avoid re-injury.
- Follow a rehabilitation plan designed by a healthcare professional.
Effective wound care is vital for athletes to maintain their active lifestyles and ensure quick recovery from injuries. The RICE method provides a solid foundation for managing acute injuries, and innovations like the Velcool® cooling and compression bandage enhance this approach. By incorporating these strategies and utilizing advanced products, athletes can minimize downtime, promote healing, and get back to their peak performance levels swiftly.
For athletes and sports enthusiasts, embracing the right wound care techniques and products like Velcool® can make a significant difference in their overall health and performance. Stay active, stay safe, and ensure your body gets the care it deserves.