How Lifestyle Choices Impact Wound Healing
Wound healing is a complex biological process involving tissue repair, immune defense, and cellular regeneration. While medical treatment plays a key role, lifestyle choices significantly influence the body’s ability to heal.
From nutrition to stress management, everyday habits can either support faster recovery or hinder the healing process.
In this blog, we explore the key lifestyle factors that impact wound healing and how simple, evidence-based changes can make a difference.
1. Nutrition: Fuel for Tissue Repair
a. Protein
- Vital for collagen formation and wound matrix development
- Protein deficiency may lead to slower wound closure and increased risk of infection
b. Vitamins and Minerals
- Vitamin C: Enhances collagen synthesis and capillary strength
- Zinc: Supports immune function and cell proliferation
- Vitamin A: Promotes epithelialization and helps control inflammation
c. Hydration
- Maintains blood volume and supports oxygen/nutrient delivery
- Dehydration can delay granulation and cell regeneration
Tip: Include lean proteins, citrus fruits, leafy greens, and zinc-rich foods like seeds and legumes in your daily meals.
2. Smoking: A Major Healing Inhibitor
Nicotine and other chemicals in tobacco constrict blood vessels, reducing oxygen supply to healing tissue.
- Impairs collagen production and fibroblast function
- Increases the risk of infection and delayed healing
- Reduces overall immune response
Quitting smoking—even temporarily during recovery—can significantly improve healing outcomes.
3. Alcohol Consumption: Delaying Recovery
Excessive alcohol intake:
- Suppresses immune function
- Depletes nutrients like Vitamin C and zinc
- Prolongs inflammation and disrupts tissue repair phases
Limit alcohol consumption to promote a healthy inflammatory response and proper wound granulation.
4. Physical Activity and Mobility
Moderate movement encourages circulation and supports healing—especially for patients at risk of pressure ulcers.
- Improves oxygenation and nutrient transport
- Reduces risk of blood pooling and edema
- Prevents pressure injuries in bedridden individuals
Regular repositioning and guided physiotherapy are essential in wound care plans.
5. Stress Management: Healing Starts with the Mind
Chronic stress elevates cortisol levels, which suppresses immune function and delays inflammatory responses crucial for wound healing.
- Impairs macrophage activity and T-cell function
- Slows tissue repair and increases infection risk
Practices like mindfulness, deep breathing, and adequate rest can accelerate recovery.
6. Chronic Conditions & Lifestyle Adjustments
Certain medical conditions magnify wound healing challenges:
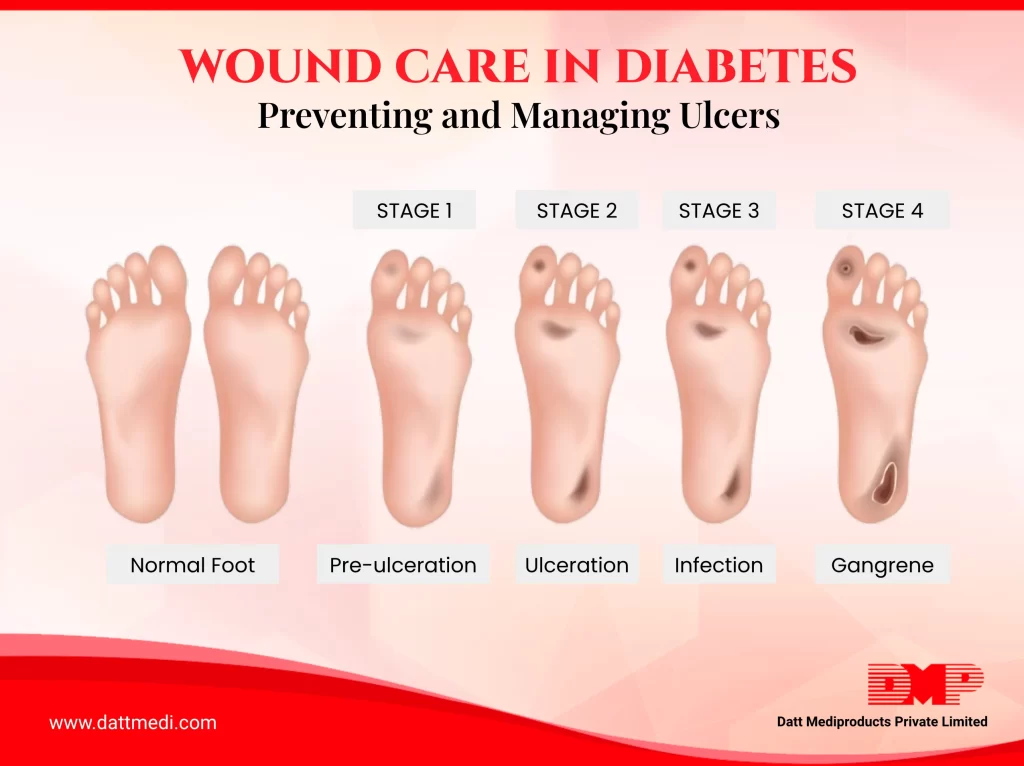
- Diabetes: High blood glucose impairs leukocyte function and circulation
- Obesity: Increased inflammation and reduced vascular flow to wound sites
Lifestyle interventions like glucose control, weight management, and routine exercise can reduce wound complications.
7. The Power of Sleep in Healing
During deep sleep, the body enters restorative phases that facilitate cell repair, hormone regulation, and immune modulation.
- Lack of sleep can delay fibroblast activation and collagen remodeling
- Poor sleep patterns are linked to chronic wound persistence
Aim for 7–9 hours of quality sleep to support recovery and immunity.
8. Wound Hygiene and Safe Practices
Proper wound care is essential for minimizing infection and supporting a moist healing environment.
- Clean wounds with prescribed solutions
- Avoid using unapproved topical agents or picking at scabs
- Use appropriate antimicrobial dressings and change them regularly
Always follow healthcare provider instructions for dressing techniques and frequency.
9. Lifestyle Checklist for Optimal Wound Healing
- Quit smoking or avoid exposure to tobacco
- Limit alcohol consumption
- Eat a balanced diet rich in healing nutrients
- Stay hydrated
- Engage in light physical activity or guided movement
- Practice stress-reduction techniques
- Get sufficient, restorative sleep
- Follow proper hygiene and wound dressing guidelines
Healing isn’t just about medicine—it’s about mindset, habits, and daily choices.
By aligning medical treatment with proactive lifestyle changes, patients can accelerate recovery, reduce complications, and regain their well-being faster.
At Datt Mediproducts, we believe in a holistic approach to healing. Our advanced wound care solutions, including antimicrobial dressings, are designed to support optimal recovery in synergy with healthy living.