Proteins are considered as the building blocks of the human body. There are several healthy reasons to make sure that we get enough protein in our diet. Protein sources include eggs, poultry, lean meat, seafood, soy products, seeds, etc.
Dairy products are also a good source of protein.
Let us discuss the goodness of PROTEIN for our bodies.
Protein Helps Build:
Protein is an integral part of building bones, muscles, cartilage, and skin. Protein helps in the formation of new cells, tissues, and other body chemicals. As a matter of fact, human hair and nails are also composed mostly of protein.
Protein Helps Repair:
The human body uses protein to build and repair tissues.
Protein Oxygenates:
The protein compound present in human RBCs helps to carry oxygen to the entire body, thereby also supplying nutrients required by cells and tissues.
Protein Helps Digest:
The protein we consume in our diets acts as a building block of enzymes that aid in digestion and boosts metabolism. Protein helps in the formation of new cells, tissues, and other body chemicals.
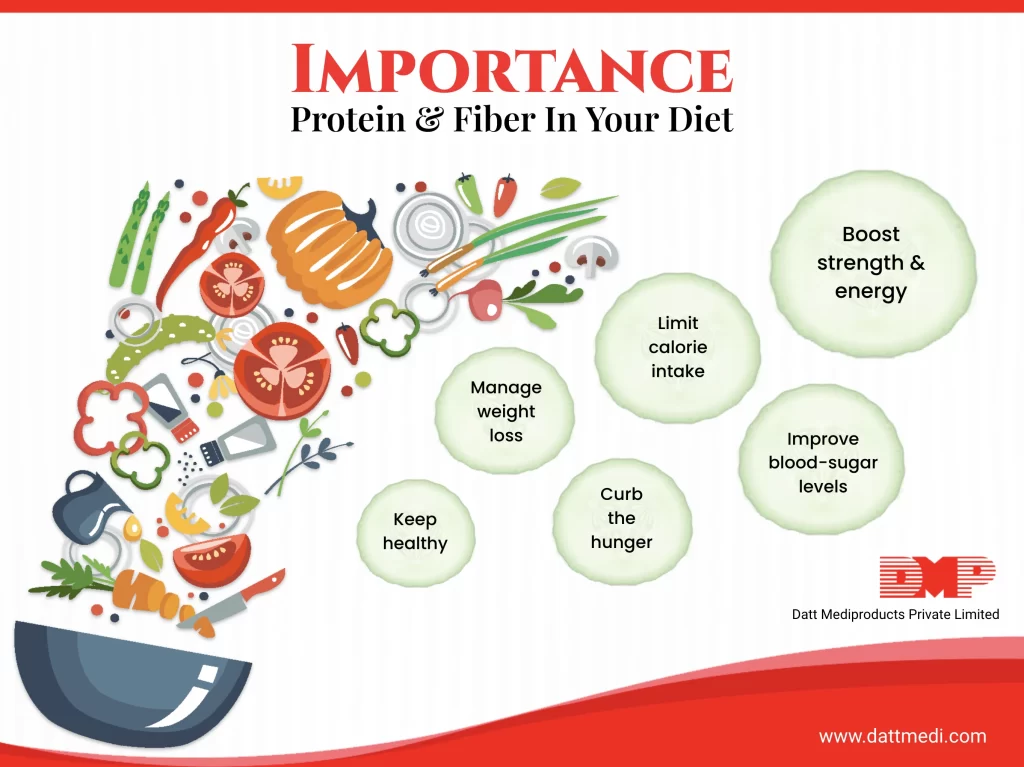
Consuming more proteins in our diet helps in losing fat and maintaining muscle mass. Protein thereby helps in weight management while supplying the right nutrients to our cells.
Protein Helps Regulate:
Protein regulates hormones especially during the transformation and development of cells during the puberty period.
Do you know our body uses extra protein for energy!
The dietary protein from plant sources provides fiber along with other health-promoting nutrients. Fiber and Protein maintain satiety level and keeps us full longer.
Let’s discuss the goodness of fiber for our bodies.
FIBERS are an essential ingredient of a healthy diet. They are best known for their ability to prevent and relieve constipation. Dietary fibers are mainly found in fruits, vegetables, legumes, and whole grains. It is often difficult to find tasty foods that contain fibers.
Let us discuss the goodness of FIBER for our bodies.
Fiber helps in Bowel Movement:
Dietary fiber softens your stool and increases its weight, making it easier to pass through the colon, thereby reducing constipation. On the other hand, fiber also adds bulk to the stool and solidifies it in diarrhea cases.
Fiber controls Blood Sugar Levels:
The soluble fibers reduce the rate of sugar absorption, thereby improves blood sugar levels. The sugar present in food rich in fiber is absorbed slower, because of which the blood glucose levels rise at a slower pace. This is good because a sudden increase in glucose levels also falls rapidly making you feel hungry very soon thereby resulting in overeating.
Fiber lowers Cholesterol Levels:
The soluble fibers present in oats, flaxseeds, and beans help lower low-density lipoprotein, or “bad,” cholesterol levels, ultimately total blood cholesterol levels.
Fiber Cleanses the Colon:
Fibers act like a scrub brush to clean out bacteria and other build-ups from the intestines and very likely to reduce the risk of colorectal cancer.
Do you know that fibers are not digested in our body, instead pass relatively intact through your stomach, small intestine, and colon and out of our body!
TIP: Drink plenty of water. A high fiber diet acts best when it absorbs water. Otherwise, too much of it may lead to abdominal bloating, cramps, and intestinal gas.
Follow us @Dattmediproducts to know more about good food choices to make.




