Overcoming Delayed Healing: Common Causes and Practical Tips
Healing is a natural process—but sometimes, wounds don’t heal as quickly as expected. Delayed healing can impact physical comfort, increase the risk of infection, and reduce quality of life.
The good news…
Many common causes of delayed healing can be managed with simple lifestyle adjustments. Let’s explore these causes and discover actionable tips for improving the healing process.
Understanding Delayed Healing
Wound healing is influenced by various factors—some within our control, others that may require professional intervention. Identifying these causes is the first step toward a faster, more efficient recovery.
Common Causes of Delayed Healing
- Poor Nutrition: Lack of essential nutrients, such as proteins, amino acids, fatty acids, carbohydrates, vitamins (A, C & E) and micronutrients (magnesium and zinc) to name a few, slows tissue repair by affecting one or more phases of the wound healing process.
- Inadequate Hydration: Dehydration impairs skin regeneration.
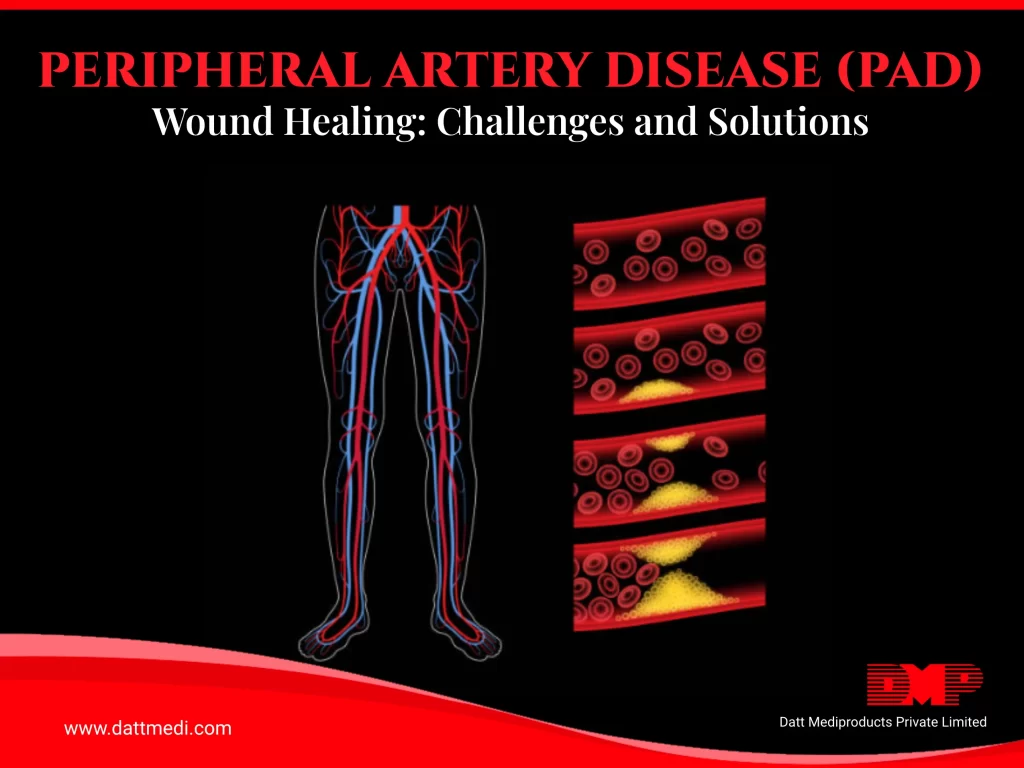
- Underlying Health Conditions: Conditions like diabetes, diabetes associated neuropathy, vascular diseases, or immune disorders can complicate healing.
- Smoking or Alcohol Consumption: These enhance host susceptibility to infections that lead to impaired angiogenesis thereby reducing blood flow and oxygen delivery to tissues which are essential for wound healing.
- Stress and Poor Sleep: Disrupt hormone balance and deregulate the immune system, which directly affects recovery. Additionally, stressed individuals are more likely to develop unhealthy habits such as inadequate nutrition, smoking, less exercise, poor sleep patterns; negatively modulating the healing mechanism.
- Infection or Repeated Trauma to the Wound: Can significantly hinder the healing process. Microorganisms obtain easy access to the underlying tissues when skin is injured. The presence of replicating microorganisms in the wound elongates the inflammatory phase of the wound healing process. This can lead to the wound to enter into a chronic state with significant delay in wound healing.
Nutrition & Hydration Matter
Proper nutrition is essential for healing.
Incorporate the following into your diet:
- Lean proteins (eggs, fish, legumes) for tissue repair
- Fresh fruits and vegetables for vitamins and antioxidants
- Whole grains to support energy levels and tissue growth
Tip: Staying well-hydrated ensures nutrients are transported to your cells, promoting faster healing and flushing out toxins.
Sleep & Stress Management
Proper rest accelerates healing. Focus on these habits:
- Aim for 7–9 hours of sleep each night.
- Practice mindfulness or relaxation techniques to reduce stress.
- Limit screen time and caffeine before bed to enhance sleep quality.
Did You Know? Chronic stress raises cortisol levels, slowing wound recovery.
Daily Movement & Gentle Activity
Physical activity promotes circulation, which helps deliver oxygen and nutrients to healing tissues:
- Engage in light activities, like short walks, if possible.
- Avoid putting pressure on the wound site, and take care to avoid friction.
- Elevate limbs to reduce swelling.
Important: Always follow your healthcare provider’s advice regarding movement and wound care.
Basic Wound Hygiene
Maintaining wound hygiene is crucial:
- Keep the wound clean and protected with proper dressings.
- Change dressings regularly, as advised by your healthcare provider.
- Avoid touching or scratching the wound area.
Pro Tip: Wash your hands thoroughly before and after touching a wound to reduce infection risk.
When to Seek Help
If your wound isn’t healing as expected or you get fever or flu-like symptoms or the wound shows signs of infection (such as increased redness, heat, swelling, pus, or a foul odor), seek professional medical guidance. Conditions like diabetes or circulatory issues may require specialized wound care.
Take Small Steps Toward Better Healing
Every small change—from better hydration to taking a short walk—adds up. By staying informed and committed to your healing process, you give your body the best chance to recover naturally.
Empowering You with the Right Solutions
At Datt Mediproducts, we understand the importance of optimal healing. While we don’t provide medical treatment, our advanced wound care solutions are designed to support your recovery by offering comfort, protection, and care where it matters most.