We all need a balanced diet to stay healthy. A Healthy Eating Food Pyramid is a guide to pick your food for healthy eating. It’s all about eating the right food in the right amount.
Eat the Right Food in the Right Amount
Different foods have distinct nutritional values. And, it is practically not possible to derive all nutrients from one particular kind of food. The Food Pyramid gives us different food groups and guides to eating a variety of foods from within each group to meet daily nutritional needs.
In addition, eating the right amount, neither too much nor too little is also important and essential for good health. Eating too little, not enough leads to under-nutrition and deficiency symptoms whereas eating too much may lead to over-nutrition and hence obesity.
Do You Know?
“The original food pyramid was created in Sweden in 1974”
The Healthy Eating Food Pyramid
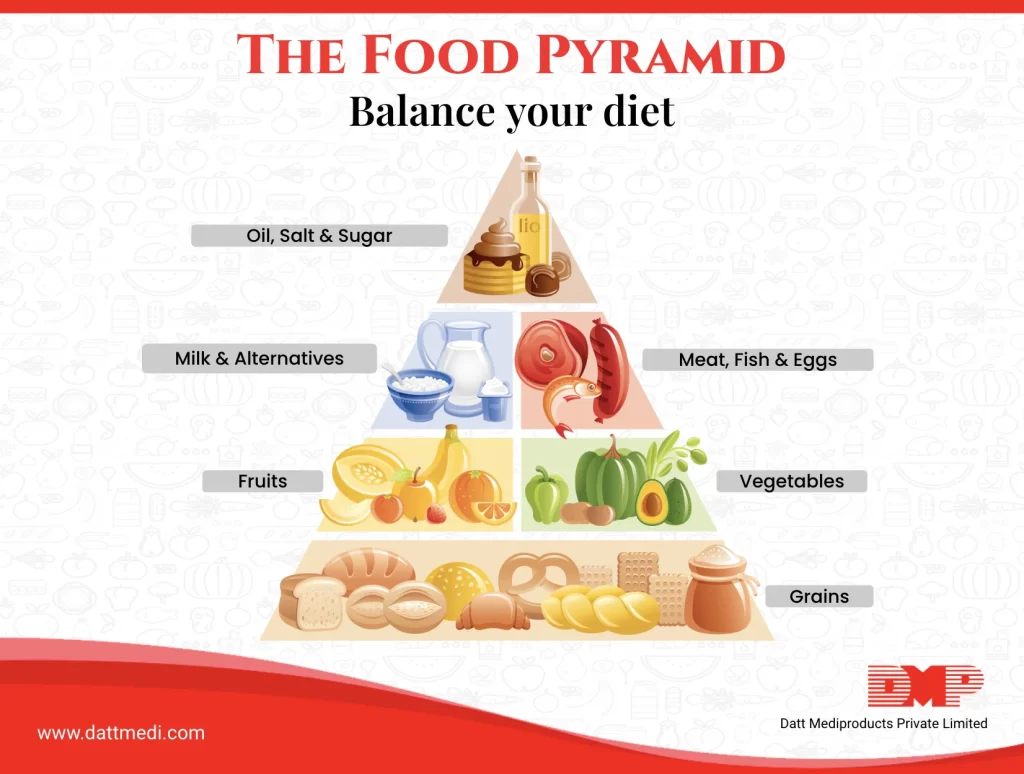
There are different shelves/levels in the healthy eating pyramid for adults, wherein different foods are organized and categorized, with the most bottom shelf as the most important one and the one on the top as the least.
Consume Adequately-
Grains, wholemeal cereals, legumes, bread, potatoes, pasta, oats, rice, etc. with 3-5 servings per day to meet your daily needs of energy. Whole Grains are the best for health. The amount depends upon your age, size, gender, and activity levels.
Eat Generously-
Vegetables, salad, and fruits with 5-7 servings per day to meet your daily dose of vitamins and minerals. A variety of colors on your plate is healthy. More is always better.
Eat Moderately-
Meat, fish, egg, yogurt, nuts, cheese, and milk with 2 servings per day to meet the daily need for proteins, calcium, and vitamin D supplements. Reduced fat or a low-fat dairy product may be chosen over the normal counterparts. Restrict oily fish consumption up to twice a week. Relish cheese in small amounts.
Eat Sparingly-
Processed foods Fat/ oil, spreads, salt, and sugar in very small amounts. Choose healthy fats/oils such as Olive, Canola, Soy, Corn, Sunflower, Peanut oils. Choose mono or polyunsaturated reduced-fat or light spreads and avoid Trans Free Margarine, mayonnaise, coleslaw, and other salad dressings that contain oil. Try to use the least amount of oil for stir-frying, baking, grilling, etc.
Drink an adequate amount of fluid (including water, tea, clear soup, etc) every day
TIP:
Foods and Drinks high in fat, sugar, and salt content are NOT meant for every day. Limit their consumption to a maximum of once or twice a week as they are not needed for good health.
The Healthy Eating Food Pyramid also inscribes the other aspects of a healthy lifestyle, such as exercise, weight management, multivitamin supplements, and controlled alcohol consumption. Thereby, we can consider this food pyramid as a very useful tool for health professionals and health educators.
We @dattmediproducts recommend adjusting the preferred foods and their amounts on an individual basis to fit your health, lifestyle, and life-stage. The aim should be a balanced meal for optimal health. Because it’s all about making smart food choices.
STAY HYDRATED as water is one of the key nutrients to maintain health and wellness.




