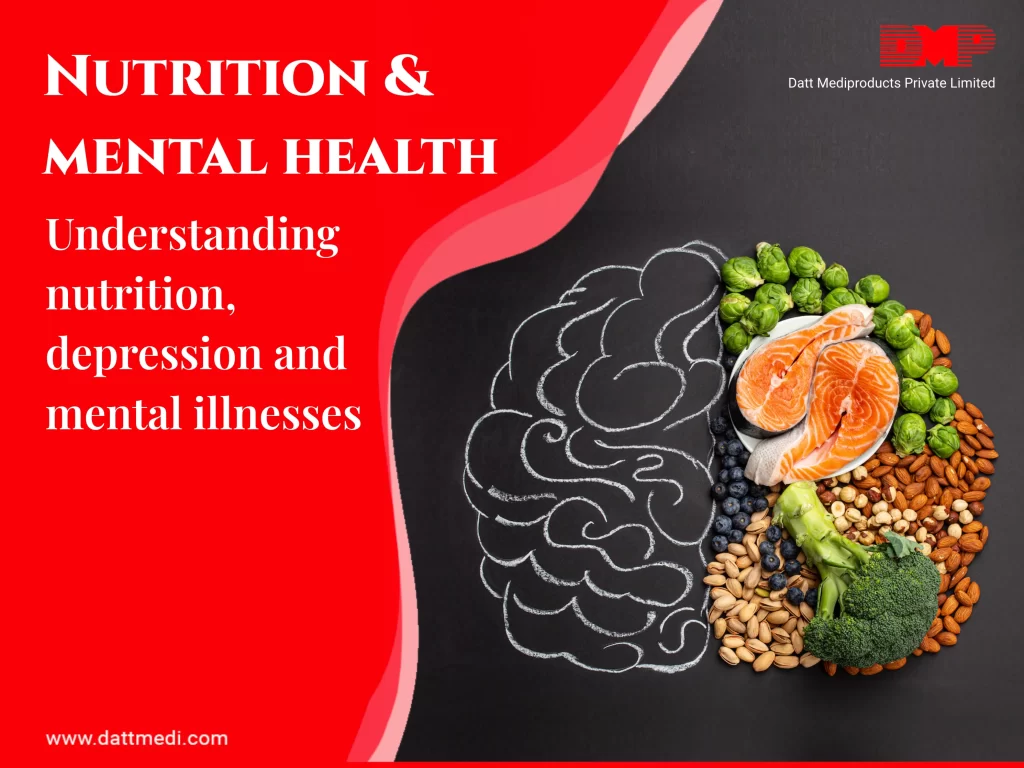
Good nutrition is essential for our physical health, but did you know it can also have a significant impact on our mental health? In recent years, researchers have discovered a strong link between what we eat and our mood, emotions, and overall mental well-being. In this blog, we’ll explore this connection in more depth and provide practical tips for how to balance both nutrition and mental health for optimal overall health.
What is Nutrition?
Nutrition refers to the process of providing the body with the essential nutrients it needs to function properly. These include carbohydrates, proteins, fats, vitamins, minerals, and water. These nutrients are essential for growth, repair, and maintenance of the body’s tissues, organs, and systems. Good nutrition is essential for maintaining good physical health and preventing chronic diseases.
The Depth of Mental Health
Mental health is a state of emotional, psychological, and social well-being. It encompasses how we think, feel, and behave, and how we interact with others. Good mental health is essential for overall well-being, and mental health disorders can have a significant impact on our daily lives, relationships, and ability to function.
The Interconnection Between Nutrition and Mental Health
Emerging research suggests that nutrition and mental health are intricately linked. Certain nutrients have been found to influence brain structure and function, impacting mood, cognition, and behaviour. For example, omega-3 fatty acids found in fatty fish, walnuts, and flaxseeds have been associated with a reduced risk of depression and improved cognitive function. Similarly, B-vitamins, such as folate and vitamin B12, play a role in the synthesis of neurotransmitters, which regulate mood and emotions. Even, a diet high in sugar and processed foods has been linked to an increased risk of depression and anxiety.
On the other hand, a diet rich in fruits, vegetables, whole grains, and lean protein can have a positive impact on mental health. Fruits, vegetables, whole grains, and lean protein are packed with essential nutrients, including vitamins, minerals, antioxidants, and fibre. These nutrients play a vital role in supporting brain health and functioning. For example, B-vitamins, found in abundance in whole grains, contribute to the production of neurotransmitters involved in regulating mood and emotions. Antioxidants, found in fruits and vegetables, help protect the brain from oxidative stress and inflammation, which can negatively impact mental health.
How to Balance Both?
Balancing both nutrition and mental health is essential for overall health and well-being. Here are some practical tips for how to do so:
1. Eat a balanced diet:
A balanced diet should include a variety of fruits, vegetables, whole grains, lean protein, and healthy fats.
2. Avoid processed foods and sugar:
Processed foods and sugar can lead to inflammation in the body, which can have a negative impact on mental health.
3. Stay hydrated:
Drinking enough water is essential for overall health, including mental health.
4. Get enough sleep:
Sleep is essential for mental and physical health. Aim for 7-9 hours of sleep each night.
5. Exercise regularly:
Exercise is a natural mood booster and can help reduce symptoms of anxiety and depression.
6. Practice self-care:
Taking time for yourself to relax and unwind can help reduce stress and improve mental well-being.
Good nutrition and good mental health are essential for overall health and well-being. Our attitude, emotions, and mental health can all be significantly impacted by what we consume. The interconnection between nutrition and mental health is complex, but by making simple changes to our diet and lifestyle, we can significantly improve our overall well-being.
We recognize the importance of taking an integrated approach to healthcare, which includes promoting good nutrition and mental health. We hope this blog has been informative and helpful in raising awareness about the link between nutrition and mental health, and inspiring individuals to take steps towards a healthier and happier life.