Vascular Access Devices (VADs) are an essential element of modern medicine and healthcare.
Vascular access devices (VADs) are inserted into veins via peripheral or central vessels for diagnostic or therapeutic reasons, such as blood sampling, central venous pressure readings, administration of medication, fluids, total parenteral nutrition (TPN) and blood transfusions.
It has been documented that about 90% of hospitalized patients require VADs, which help in the administration of medications, fluids, nutrition, and monitoring & diagnostics. Although the insertion of such devices has become a routine procedure, much importance is not given to the securement techniques and dressings.
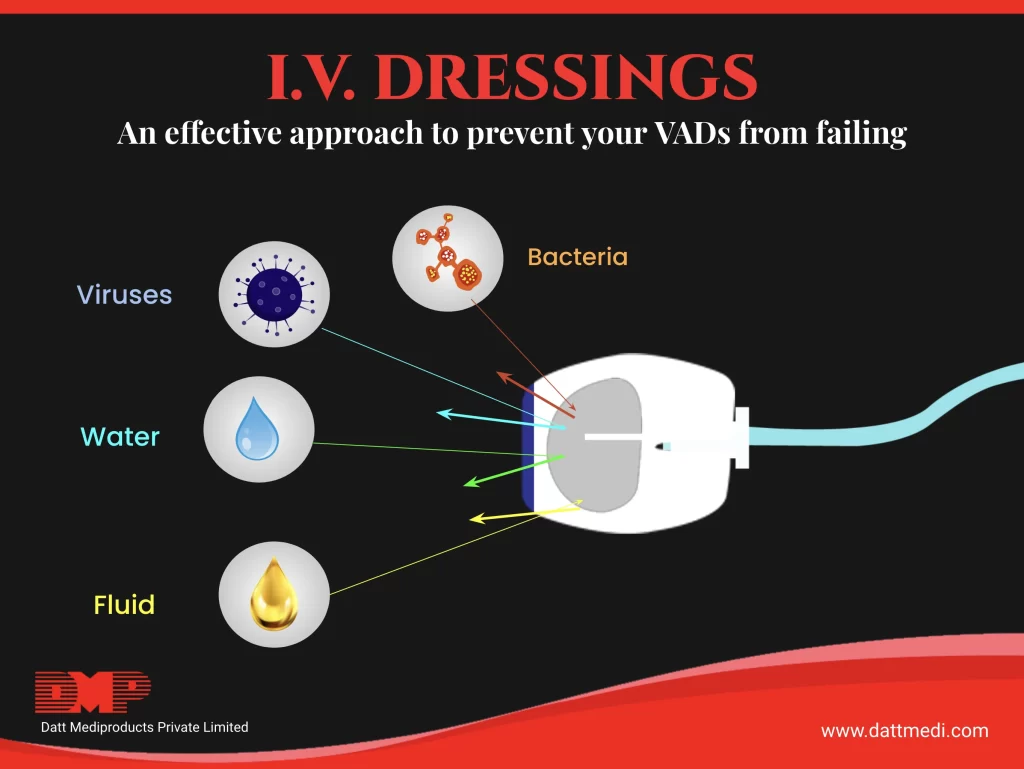
There are a range of wound dressings and securement devices available used for VAD stabilization. These may include sterile gauze/tape, transparent dressings, antimicrobial dressings, and sutureless securement dressings. Let us discuss IV Dressings as a securement device for VADs in detail.
What are IV Dressings?
IV Dressings are used to secure catheters and IV cannula to the insertion point. These are mostly transparent in nature. IV dressings allow moisture and oxygen transmission while maintaining a slightly damp wound healing environment. These dressings are impermeable to bacteria, germs, and other external contaminants. Thus, these dressings help to maintain a clean and dry catheter site by blocking the germs.
Properties of IV Dressings
- Conformable
- Waterproof, allows the patients to shower
- Permeable to moisture vapor and oxygen
- Impermeable to external contaminants
- Effective wear time of up to 7 days
- Mostly transparent in nature allowing continuous observation
- Available in a variety of thicknesses and sizes
Benefits of IV Dressings
- Provide a barrier to external contaminants: Using a sterile gauze to secure an IV dressing doesn’t provide the barrier against external contaminants. On the other hand, transparent IV dressings are advantageous as these allow an effective impermeable environment to the microorganisms, still being permeable to the water vapours and the oxygen.
- Daily Observation: Transparent IV dressings offer an additional advantage of daily continuous observation without removing the dressing.
- Reduced number of Dressings: Gauze and Tapes need to be changed after every 2 days. The skin may become fragile by repeated dressing changes and this could further damage the skin. On the other hand, transparent IV dressings can be used for up to 7 days.
- Patient Compliance: Less frequent dressing changes offer increased patient comfort. It also helps to maintain skin integrity and lowers the risk of infection and trauma.
- Cost Effective: Historically, gauze and tapes were perceived as an inexpensive option over the transparent IV dressings. Nowadays, it has been observed that the cost may be comparable if the therapy continues for more than 3 days.
- Additional Benefits: Transparent IV dressings available with additional securement options offer a better stabilization of the catheter, reduce the risk of dislodgement, better wear time and fewer chances of infections.
Indications
- IV Cannula Fixation
- Catheter sites
Changing an IV Dressing
- Changing an IV Dressing at regular intervals is important. An average dressing change time is 3 to 5 days, these dressings though have an advantageous wear time of up to 7 days.
- Changing the dressing also keeps bacteria and germs away from the catheter site, thus reducing the risk of infections.
- The dressing must be changed if any kind of redness or irritation is observed, or if the dressing gets loosened, wet or dirty or if any leakage is present.
Other Considerations
- Because of the adhesive nature of an IV dressing, its transparent film won’t adhere to a moist surface.
- Transparent IV dressings are contraindicated in patients who have moderate to heavy exudates, infection, third-degree burns etc.
- These dressings are not recommended for patients with fragile or thin skin, for example, old age patients. An epidermal stripping or skin tears may also be seen in patients on steroids.
We @ Datt Mediproducts Pvt. Ltd. manufacture and market a range of
I.V. dressings with impeccable quality following international standards.
Our I.V. dressings offer a transparent, waterproof film which acts as a bacterial barrier, yet are breathable.
The Dressings are available with a unique coat technology offering high MVTR (moisture vapour transmission rate). Latex-free and hypoallergenic adhesive is used which gently adheres to the skin and offers an easy removal. Our dressings ensure gentle and effective securement while delivering constant adhesive strength. For more info on our IV dressings, visit www.dattmedi.com or contact us at info@dattmedi.com.