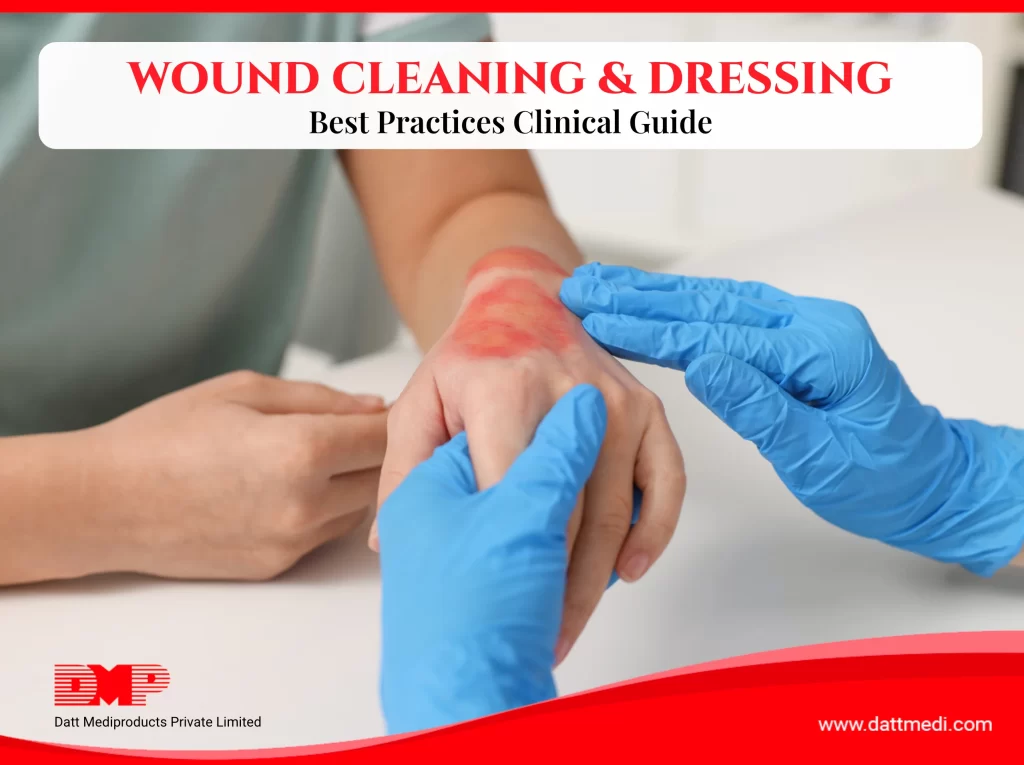
Knowing how to clean a wound properly and apply the right dressing plays a critical role in healing outcomes. Inadequate wound care is one of the most common reasons wounds become infected or take longer to heal.
Whether managing a minor cut at home, caring for a surgical incision, or supporting chronic wound recovery, following evidence-based wound care practices helps protect the skin, reduce complications, and support natural tissue repair.
Why Proper Wound Care Is Important
Proper wound care involves cleaning the wound, protecting it with an appropriate dressing made from clinically tested materials, and regularly monitoring the healing progress.
Effective wound care:
- Reduces microbial contamination
- Minimizes inflammation and tissue damage
- Lowers the risk of scarring and delayed healing
- Supports tissue regeneration, especially in patients with diabetes, poor circulation, or reduced immunity
Maintaining a clean and protected wound environment allows new tissue to form safely and consistently.
Practical example:
Healthcare facilities worldwide follow standardized wound care protocols because consistent and correct wound management directly improves patient recovery outcomes.
Step-by-Step Guide: How to Clean a Wound
A. Prepare Before Cleaning the Wound
1. What to do:
Prepare yourself and gather supplies before touching the wound.
2. Why it matters:
Proper preparation minimizes the risk of introducing bacteria into the wound.
3. How to do it:
- Wash hands thoroughly and wear clean gloves.
- Keep sterile saline or clean water ready.
- Prepare clean, suitable wound dressings as advised, along with a waste disposal bag.
B. Clean the Wound Gently and Safely
1. What to do:
Remove visible dirt, debris, or dried discharge from the wound.
2. Why it matters:
Gentle cleaning reduces infection risk and supports faster healing.
3. How to do it:
- Rinse the wound using a mild soap and sterile saline or clean running water
- Use antiseptic solutions only if recommended by a healthcare professional
- Avoid alcohol or hydrogen peroxide directly on the wound, as these may damage healthy tissue and delay healing
C. Dry the Wound Area Carefully
1. What to do:
Dry the surrounding skin after cleaning.
2. Why it matters:
Excess moisture can weaken surrounding skin and slow healing.
3. How to do it:
- Gently pat the area dry using sterile gauze
- Avoid rubbing the wound surface
Choosing the Best Dressing for Open Wounds
A. Factors to Consider When Selecting a Dressing
The best dressing for open wounds depends on:
- Type of wound (minor cut, surgical incision, or chronic wound)
- Amount of wound exudate (fluid)
- Infection risk and patient activity level
Selecting the right dressing—based on wound type and healing needs—helps maintain an optimal wound environment and supports steady healing.
B. Common Types of Wound Dressings and Their Uses
- Gauze Dressings:
Suitable for minor wounds and short-term protection, such as Gamjee pads and cotton gauze rolls. - Foam Dressings:
Ideal for moderate to heavily exuding wounds, such as Velfix-S, which helps absorb excess exudate while maintaining a balanced wound environment. - Hydrocolloid or Hydrogel Dressings:
Help maintain a moist environment for healing. - Antimicrobial Dressings:
Recommended when infection risk is high or infection is present, such as Velvert, used under medical guidance.

Modern wound management relies on advanced dressing technologies designed to maintain moisture balance and protect healing tissue. – Read More
How to Secure a Wound Dressing Correctly
1. Why it matters:
A dressing that is too loose may expose the wound, while one that is too tight can restrict circulation.
2. Best practices:
- Use transparent sterile film dressings (Velfix-T Film) to secure the primary dressing while allowing wound visibility.
- Medical adhesive tape may be used where appropriate.
- Ensure the dressing is secure, comfortable, and does not restrict blood flow.
How Often Should You Change a Wound Dressing?
Dressing change frequency depends on wound type, exudate level and medical advice. Change the dressing if:
- It becomes wet or contaminated
- There is increased redness, discharge, or odor
- Wounds with higher exudated will require more frequent dressing changes.
Regular dressing changes using clean and sterilized post-operative or wound dressings reduce infection risk and support faster healing.
Monitoring Wound Healing and Infection Signs
Check the wound daily for:
- Increased pain, redness, swelling, or warmth.
- Discharge or unusual odor (possible infected wound signs).
- Healthy pink or red tissue, which indicates healing.
If healing does not improve or symptoms worsen, consult a healthcare professional promptly.
If any warning signs persist or worsen, early identification is critical. Understanding the common symptoms of wound infection can help prevent serious complications and delayed healing.

Read more: Signs of Infected Wounds: Symptoms, Risks, and When to Seek Medical Care
Common Wound Care Mistakes to Avoid
- Using non-sterile or unclean materials
- Leaving wounds uncovered for extended periods
- Reusing old or soiled dressings
- Applying products without professional advice
Avoiding these mistakes can significantly improve recovery outcomes.
When to Seek Medical Attention for a Wound
Seek professional care if:
- The wound is deep or bleeding heavily
- It is a burn
- Signs of infection are present
- The wound is chronic, such as diabetic foot ulcers or burns
- Healing does not progress over time
In such cases, specialized solutions like advanced wound dressings may be required, under the guidance of healthcare professionals.
Simple Tips to Support Faster Wound Healing
- Eat a balanced diet rich in protein, vitamins, and minerals
- Stay adequately hydrated
- Avoid smoking and excessive alcohol intake
- Get sufficient sleep to support tissue repair
Understanding how to clean a wound and apply the correct dressing is essential for safe and effective healing. By following approapriate wound care steps and using quality wound dressings manufactured under international standards such as ISO and CE, patients and caregivers can reduce complications and support better outcomes.
For complex or slow-healing wounds, timely medical guidance remains essential.
Medical Disclaimer
This content is intended for general wound care education and does not replace professional medical advice. Always consult a healthcare provider for serious, worsening, or non-healing wounds.