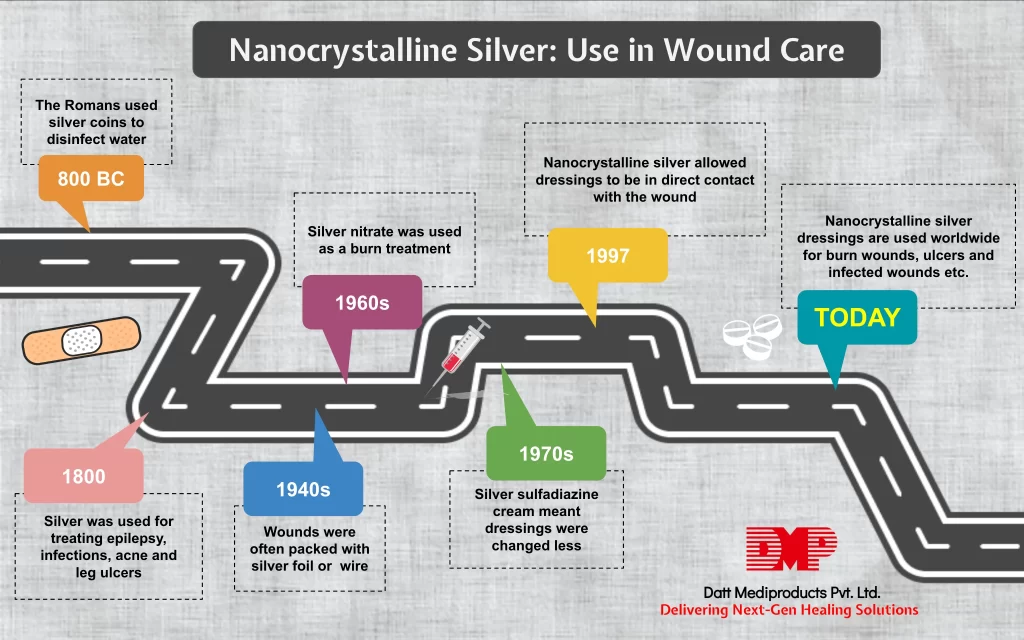
Silver has been used as an antimicrobial since the 1800s. But since the discovery of systemic antibiotics in the early 20th century, the use of silver had declined. In the last two decades, interest in silver for wound treatment has resurged. However, there are very few quantitative data available on the systemic absorption of silver and the associated clinical risk.
Let’s check out the latest product introduced, Nanocrystalline Silver and it’s applications in wound care.
What is Nanocrystalline Silver?
Nanomaterials are often unique, differing in physical, chemical and biological ways from their macro counterparts. In the case of silver, the smaller the particle the larger the surface area that is available for interaction, resulting in an increased bactericidal effect.
Nanocrystalline Silver has been introduced to the wound care industry quite recently. It’s ability to reduce bacterial count/load, is thought to be due to its possible interaction with the plasma membrane and binding with cytoplasmic protein. The dressing has got amazing disinfecting properties and heals the wounds faster than any other available dressings. Usually, people who need fast recovery from their wounds should opt for these kinds of dressings.
What wounds can Nanocrystalline Silver dressings heal?
They are known to heal any kind of burn wounds. It is also helpful for healing wounds that are chronic, infected wounds, bed sores, leg or pressure ulcers and skin grafting. As opposed to the common belief, it is non-toxic, and the silver released into the wound is controlled, so as not to cause any kind of irritation.
What are the benefits of using Nanocrystalline Silver Products?
- Fast solution and is long lasting.
- Prevents any kind of wound contamination.
- Kills all microorganism in less time.
- Versatile can be cut into any shape desired.
- Doesn’t need to be changed frequently.
- Is a cost-effective product.
Nowadays, clinicians are increasing in the use of nanocrystalline silver dressings for wound management either for their antimicrobial or anti-inflammatory properties.
We at Datt Mediproducts manufacture an international quality nanocrystalline silver dressing that has various beneficial features such as:
- It can provide a really strong barrier for microbes that last for as many as 5 days.
- It maintains the perfect moist environment required by the wound to heal.
- It is gamma sterilized and manufactured with high-quality control standards.
- It is effective against various types of highly resistant bacteria such as VRE, MRSA, etc.
For any kind of further information mail us with any questions digital.marketing@dattmedi.com and we will be happy to answer or you can visit our website www.dattmedi.com




