Discover Informative Blogs on Healthcare Solutions
Search by Blog
Read by Category
Patient Care Solutions
Health & Wellness
Environmental Health
First Aid & Emergency Care
Advance Wound Care
Wound Care
Your healing journey continues beyond this blog
Find the right products for better recovery at online store

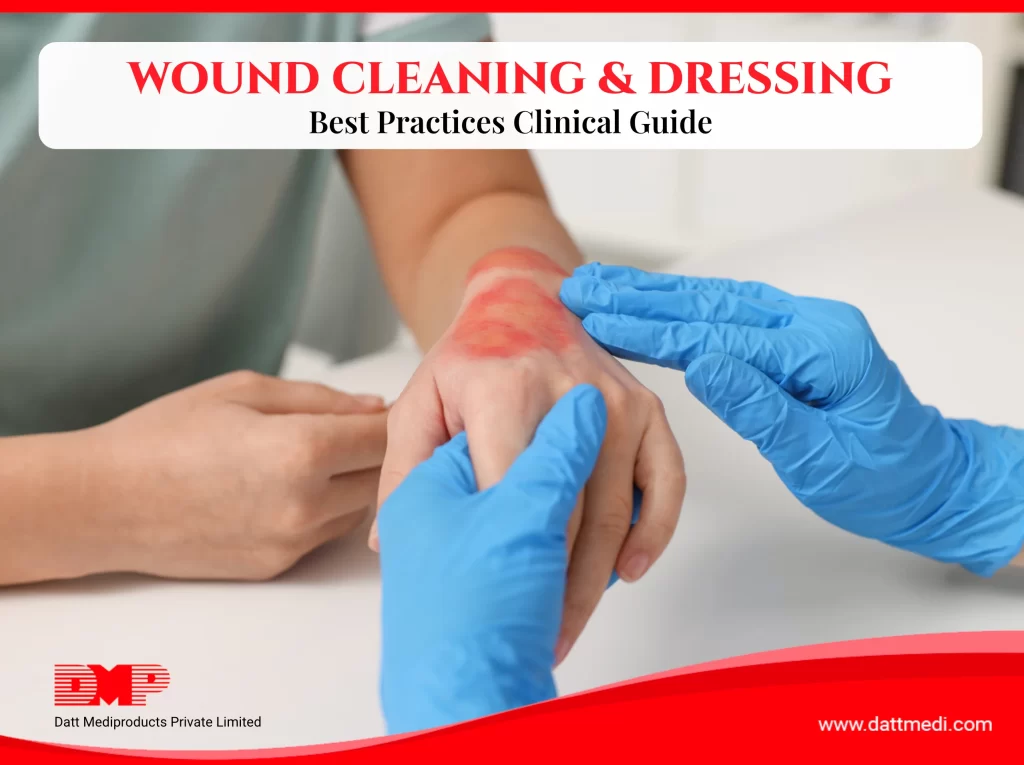
Knowing how to clean a wound properly and apply the right dressing plays a critical role in healing outcomes. Inadequate wound care is one of the most common reasons wounds become infected or take longer to heal.
Whether managing a minor cut at home, caring for a surgical incision, or supporting chronic wound recovery, following evidence-based wound care practices helps protect the skin, reduce complications, and support natural tissue repair.
Why Proper Wound Care Is Important
Proper wound care involves cleaning the wound, protecting it with an appropriate dressing made from clinically tested materials, and regularly monitoring the healing progress.
Effective wound care:
- Reduces microbial contamination
- Minimizes inflammation and tissue damage
- Lowers the risk of scarring and delayed healing
- Supports tissue regeneration, especially in patients with diabetes, poor circulation, or reduced immunity
Maintaining a clean and protected wound environment allows new tissue to form safely and consistently.
Practical example:
Healthcare facilities worldwide follow standardized wound care protocols because consistent and correct wound management directly improves patient recovery outcomes.
Step-by-Step Guide: How to Clean a Wound
A. Prepare Before Cleaning the Wound
1. What to do:
Prepare yourself and gather supplies before touching the wound.
2. Why it matters:
Proper preparation minimizes the risk of introducing bacteria into the wound.
3. How to do it:
- Wash hands thoroughly and wear clean gloves.
- Keep sterile saline or clean water ready.
- Prepare clean, suitable wound dressings as advised, along with a waste disposal bag.
B. Clean the Wound Gently and Safely
1. What to do:
Remove visible dirt, debris, or dried discharge from the wound.
2. Why it matters:
Gentle cleaning reduces infection risk and supports faster healing.
3. How to do it:
- Rinse the wound using a mild soap and sterile saline or clean running water
- Use antiseptic solutions only if recommended by a healthcare professional
- Avoid alcohol or hydrogen peroxide directly on the wound, as these may damage healthy tissue and delay healing
C. Dry the Wound Area Carefully
1. What to do:
Dry the surrounding skin after cleaning.
2. Why it matters:
Excess moisture can weaken surrounding skin and slow healing.
3. How to do it:
- Gently pat the area dry using sterile gauze
- Avoid rubbing the wound surface
Choosing the Best Dressing for Open Wounds
A. Factors to Consider When Selecting a Dressing
The best dressing for open wounds depends on:
- Type of wound (minor cut, surgical incision, or chronic wound)
- Amount of wound exudate (fluid)
- Infection risk and patient activity level
Selecting the right dressing—based on wound type and healing needs—helps maintain an optimal wound environment and supports steady healing.
B. Common Types of Wound Dressings and Their Uses
- Gauze Dressings:
Suitable for minor wounds and short-term protection, such as Gamjee pads and cotton gauze rolls. - Foam Dressings:
Ideal for moderate to heavily exuding wounds, such as Velfix-S, which helps absorb excess exudate while maintaining a balanced wound environment. - Hydrocolloid or Hydrogel Dressings:
Help maintain a moist environment for healing. - Antimicrobial Dressings:
Recommended when infection risk is high or infection is present, such as Velvert, used under medical guidance.

Modern wound management relies on advanced dressing technologies designed to maintain moisture balance and protect healing tissue. – Read More
How to Secure a Wound Dressing Correctly
1. Why it matters:
A dressing that is too loose may expose the wound, while one that is too tight can restrict circulation.
2. Best practices:
- Use transparent sterile film dressings (Velfix-T Film) to secure the primary dressing while allowing wound visibility.
- Medical adhesive tape may be used where appropriate.
- Ensure the dressing is secure, comfortable, and does not restrict blood flow.
How Often Should You Change a Wound Dressing?
Dressing change frequency depends on wound type, exudate level and medical advice. Change the dressing if:
- It becomes wet or contaminated
- There is increased redness, discharge, or odor
- Wounds with higher exudated will require more frequent dressing changes.
Regular dressing changes using clean and sterilized post-operative or wound dressings reduce infection risk and support faster healing.
Monitoring Wound Healing and Infection Signs
Check the wound daily for:
- Increased pain, redness, swelling, or warmth.
- Discharge or unusual odor (possible infected wound signs).
- Healthy pink or red tissue, which indicates healing.
If healing does not improve or symptoms worsen, consult a healthcare professional promptly.
If any warning signs persist or worsen, early identification is critical. Understanding the common symptoms of wound infection can help prevent serious complications and delayed healing.

Read more: Signs of Infected Wounds: Symptoms, Risks, and When to Seek Medical Care
Common Wound Care Mistakes to Avoid
- Using non-sterile or unclean materials
- Leaving wounds uncovered for extended periods
- Reusing old or soiled dressings
- Applying products without professional advice
Avoiding these mistakes can significantly improve recovery outcomes.
When to Seek Medical Attention for a Wound
Seek professional care if:
- The wound is deep or bleeding heavily
- It is a burn
- Signs of infection are present
- The wound is chronic, such as diabetic foot ulcers or burns
- Healing does not progress over time
In such cases, specialized solutions like advanced wound dressings may be required, under the guidance of healthcare professionals.
Simple Tips to Support Faster Wound Healing
- Eat a balanced diet rich in protein, vitamins, and minerals
- Stay adequately hydrated
- Avoid smoking and excessive alcohol intake
- Get sufficient sleep to support tissue repair
Understanding how to clean a wound and apply the correct dressing is essential for safe and effective healing. By following approapriate wound care steps and using quality wound dressings manufactured under international standards such as ISO and CE, patients and caregivers can reduce complications and support better outcomes.
For complex or slow-healing wounds, timely medical guidance remains essential.
Medical Disclaimer
This content is intended for general wound care education and does not replace professional medical advice. Always consult a healthcare provider for serious, worsening, or non-healing wounds.

At-home wound care plays a bigger role in healing than most people realize. Many wounds that later become infected or heal slowly don’t start as serious injuries; they worsen because of small, everyday mistakes in home care.
These mistakes are rarely intentional. They usually occur due to confusion, over-cleaning, ignoring signs of infection or using unsuitable dressings. With the right approach, however, effective wound care at home can significantly reduce infection risk, improve comfort, and support faster healing.
This blog is especially helpful for individuals managing minor cuts, post-surgical wounds, or caring for elderly patients at home. It explains the most common at-home wound care mistakes, how to avoid them, and when professional medical help is necessary.
Common At-Home Wound Care Mistakes (And What Works Better)
1. Over-Cleaning the Wound
The Mistake
Cleaning the wound too frequently or using strong solutions such as spirit, iodine, or hydrogen peroxide.
Why This Is a Problem
While cleaning is essential, over-cleaning can damage newly forming tissue and slow the body’s natural healing process. Repeated use of harsh antiseptics may irritate the wound bed and delay recovery.
What to Do Instead
- Always wash your hand thoroughly first
- Clean once daily or if the dressing gets dirty
- Use a mild soap and clean water or saline
- Gently pat dry—do not scrub
Practical Insight
For most minor wounds, gentle cleaning combined with appropriate wound care dressings is sufficient to prevent infection and support healthy healing.
2. Touching the Wound or Dressing Surface
The Mistake
Directly touching the wound or the surface of the dressing that comes in contact with the skin.
Why This Increases Infection Risk
Hands naturally carry bacteria, even after washing. Touching sterile surfaces can transfer germs directly to the wound, increasing the risk of infection.
What to Do Instead
- Wash hands before and after wound care
- Handle dressings only from the edges
- Avoid reusing or adjusting used dressings
Practical Insight
Using sterile ready-to-use dressings helps maintain hygiene and reduces unnecessary handling during home care.
3. Using the Wrong Dressing for the Wound
The Mistake
Applying any available bandage without considering the wound type, size, or location.
Why This Slows Healing
An unsuitable dressing may stick to the wound, trap excess moisture, irritate surrounding skin, or restrict movement—leading to discomfort and delayed healing.
What to Do Instead
- Asses the wound.
- Depending on the type of wound choose an appropriate dressing. If you need help choosing a dressing or have any doubts of the type of wound please contact a healthcare professional.
- Choose sterile, breathable, non-irritating dressings
- Ensure secure but comfortable placement
- Change the dressing regularly and if it becomes wet, dirty, or loose
Practical Insight
Well-designed gauze-based dressings and post-operative film dressings support protection, comfort, and consistent healing at home.
Step-by-Step: Safe Wound Care at Home
Following a simple routine helps prevent infection and supports steady healing.
Step 1: Assess the wound
- Assess the wound to see how serious and what type of wound it is.
- You should seek professional care if:
- you can see the bone or blood vessels
- the bleeding doesn’t stop even after pressure is applied
- it is a burn wound
- it is a bite wound from an animal
Step 2: Prepare
- Wash hands thoroughly
- Keep all dressing materials ready
Step 3: Clean
- Rinse the wound gently with mild soap and clean water or saline
- Pat dry with sterile gauze such as cotton gauze products
Step 4: Dress
- If it is a minor cut of scrape let it air out, it doesn’t need a bandage
- For larger wounds apply a sterile dressing without touching the pad
- Smooth it gently so it stays in place
Step 5: Observe
- Check and clean the wound daily. Monitor for changes
- Replace the dressing as needed

For a more detailed look at everyday care practices that help wounds heal faster, see our wound care dos and don’ts for faster healing guide.

Warning Signs: When to Seek Medical Help
At-home wound care may not be enough if you notice:
- Increasing redness, swelling, or warmth
- Yellow or green discharge
- Persistent pain or fever
- A wound that does not improve after a few days
Early medical attention can prevent serious complications and support timely recovery.
Making At-Home Wound Care Safer and Simpler
Many households prefer sterile wound care solutions because they reduce guesswork and handling. These solutions are designed to:
- Support hygiene
- Reduce infection risk
- Simplify daily wound care routines
Such products are commonly used in hospitals and home-care settings and are manufactured following international quality standards such as ISO and CE, making them trusted across global healthcare markets.
Effective wound care at home is about balance—cleaning gently, protecting properly, and knowing when professional care is needed. By avoiding common mistakes and following simple, hygienic steps, healing outcomes can be significantly improved.
With the right approach and reliable advanced wound care products, healing at home can be safe, comfortable, and confident.
Medical Disclaimer
This content is intended for general wound care education and does not replace professional medical advice. Always consult a healthcare provider for serious, worsening, or non-healing wounds.
A well-fitted compression garment supports movement, reduces swelling, and improves overall comfort during recovery. Even small measurement errors can affect its effectiveness. Whether you are a patient, caregiver, clinician, or distributor, understanding how to measure compression garments correctly ensures safe therapy and reliable results.
For suitable options, check our Compression Stockings Collection.
1. Why the Right Measurement and Fit Matters
Compression garments apply controlled pressure along the limb. The correct size ensures even pressure distribution and therapeutic effectiveness.
Benefits of Proper Fit:
- Reduces swelling and discomfort
- Improves blood and lymph circulation
- Supports healing after injury, surgery, or chronic conditions
- Makes daily activities like walking, standing, or sitting more comfortable
Example: Someone managing mild swelling or early varicose veins often feels lighter and more supported when using a properly sized garment, following a reliable compression stocking size guide.
2. Tools You Need for Accurate Measurement
Accurate sizing doesn’t require advanced tools.
You need:
- A soft measuring tape
- Manufacturer’s compression measurement chart or sizing guide
- Notebook or phone to record values
- Mirror or assistance for hard-to-reach areas
- Good lighting for accurate readings
These simple tools help follow a medical compression garment sizing guide and reduce measurement errors.
3. Step-by-Step Guide: How to Measure Correctly
i) Ankle: Measure the narrowest point above the ankle bone.
ii) Calf: Measure the widest part of the calf for proper fit and support, including wide-calf users.
iii) Thigh (for thigh-high garments): Measure the thickest part of the thigh to avoid rolling and ensure secure fit.
Leg Length:
- Knee-high: heel to just below the knee crease
- Thigh-high: heel to the top of the thigh

iv) Arms (for sleeves/supports): Measure wrist, forearm, upper arm, and arm length. This ensures smooth, even compression from wrist to shoulder.
Quick Tips:
- Measure early in the morning when swelling is minimal.
- Sit comfortably, keep tape snug, measure twice, and avoid measuring over clothes.
4. Common Fitting Mistakes to Avoid
- Too Tight: Can cause numbness, tingling, or deep marks.
- Too Loose: Slipping or wrinkling reduces effectiveness.
- Incorrect Length: Too short rolls or digs in; too long bunches or slides down.
- Not Rechecking: Limb size changes due to swelling, healing, or weight changes—regular measurement is important.
For reference, see our Compression Stockings Size Chart India.
5. When to Consult a Healthcare Professional
Specialists can confirm the correct compression level and ensure measurements match your condition, especially after surgery or for vascular issues.
Consult if you notice:
- Persistent or increasing swelling
- Discomfort while wearing the garment
- Size falling between two chart options
- Post-surgical changes
- Conditions like diabetes or vascular disorders
Professional guidance ensures safe and effective therapy, particularly when using compression garments for varicose veins.
Accurate measurements are the foundation of effective compression therapy. Using simple tools, careful technique, and a trusted compression stocking size guide ensures your garment fits comfortably and supports healing. When unsure, consulting a healthcare professional provides confidence and safer results.

Wound healing is often slowed when the body cannot efficiently move blood and excess fluid away from the affected area. This causes low blood flow which leads to reduced oxygen & nutrient supply, both are critical for cell repair. This is frequently seen in chronic venous ulcers, lymphedema, diabetic wounds, and post-surgical swelling.
Compression therapy is one of the most effective clinical methods to improve circulation, support healing, and enhance overall wound management.
By applying controlled and consistent pressure, compression therapy reduces fluid buildup, improves oxygen delivery, and creates a stable environment that promotes faster tissue repair.
What Is Compression Therapy? How It Works
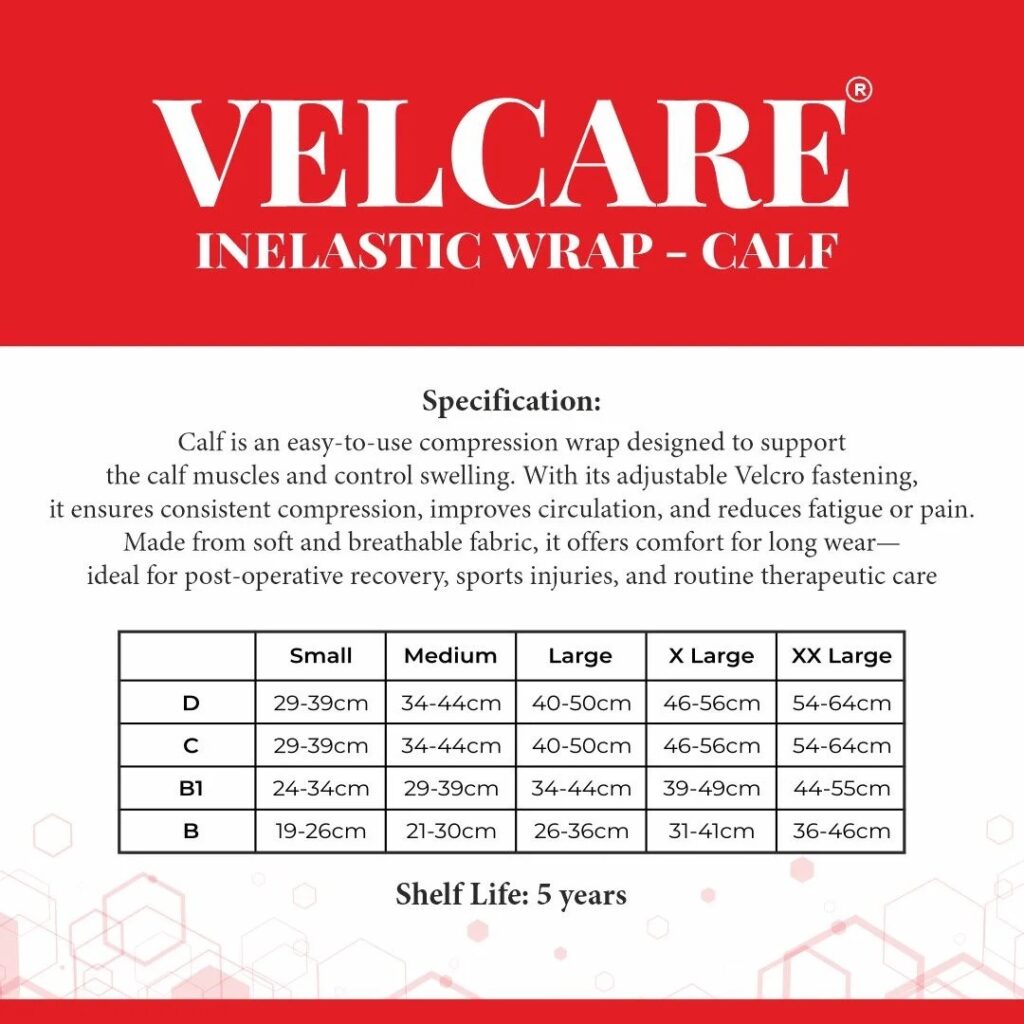
Compression therapy uses medical tools such as compression bandages, garments, or dressings to apply even pressure to a limb or wound site. This helps to:
- Redirect blood flow toward the heart
- Reduce fluid accumulation under the skin
- Improve oxygen supply to damaged tissues
- Support formation of healthier new tissue
This controlled pressure creates a stable, balanced healing environment and reduces strain on surrounding skin.
Types of Compression Therapy
1. Elastic Compression Bandages
Widely used for venous ulcers and chronic wounds because they allow adjustable pressure and support daily wound care.
Related Product: Compression Bandages – Wound Care Range
2. Compression Garments
Ideal for long-term swelling, lymphedema care, and post-surgical recovery. They offer uniform pressure and help maintain inflammation control. Velcare® Varicose Vein Stockings– Compression Garments
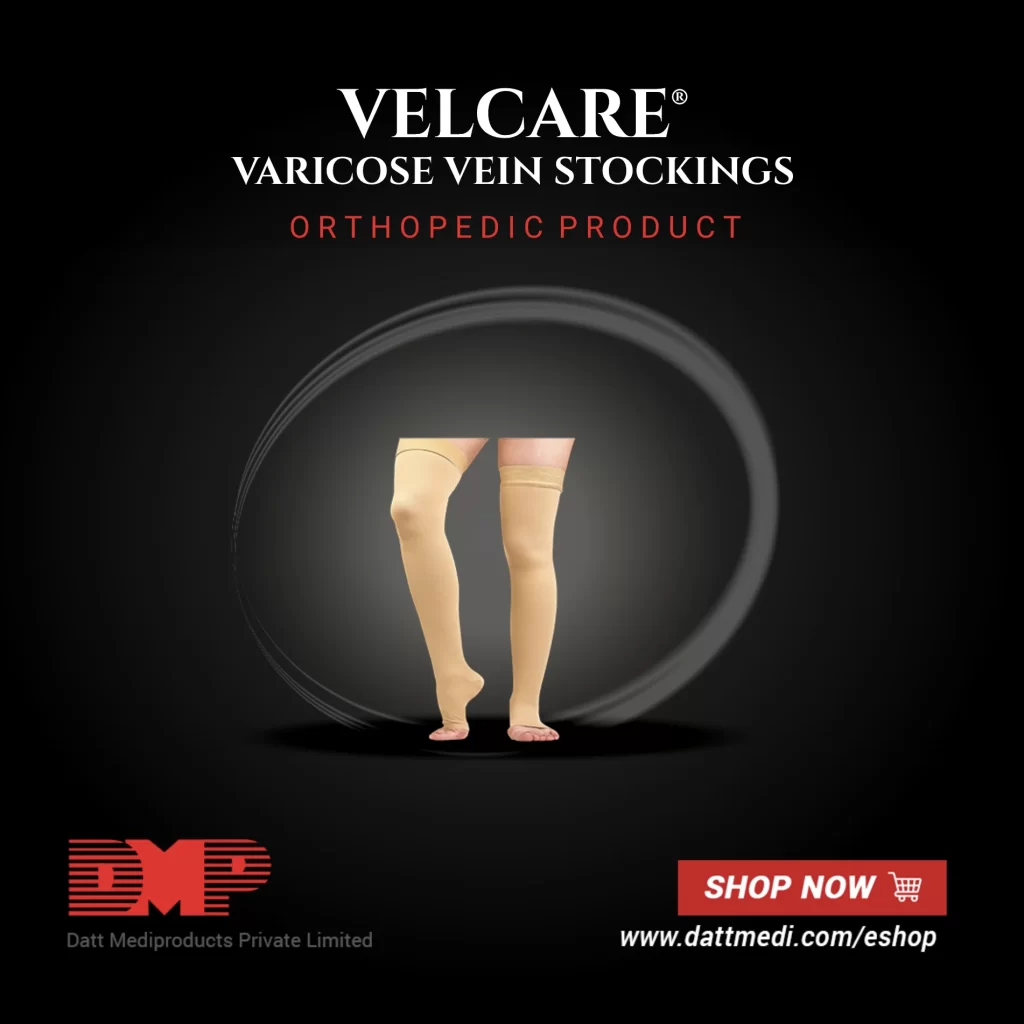
Know More About – Velcare® Varicose Vein Stockings- Compression Garments
3. Dressings With Built-In Mild Compression
Foam and hydrocolloid dressings provide gentle compression while maintaining moisture balance. Recommended options:
- Velfix® Foam Dressings – Advanced Wound Care
- Velsoft® Silicone Foam Dressings – Advanced Wound Care
- Velvert® Advanced Dressings – Antimicrobial & Moisture Management
How Compression Therapy Supports Wound Healing
- Improved Blood Flow – Prevents blood pooling and delivers oxygen and nutrients for efficient tissue repair.
- Swelling Control (Edema Management) – Removes trapped fluid, reducing discomfort and creating a stable environment.
- Enhanced New Tissue Formation – Supports orderly tissue repair and faster wound closure.
- Reduced Risk of Raised Scars – Mild compression after surgery or burns helps prevent thick or raised scars.
When Compression Therapy Is Recommended
- Chronic Venous Ulcers – Supports circulation and long-term healing.
- Lymphedema Care – Manages fluid buildup, heaviness, and infection risk.
- Post-Surgical Recovery – Controls inflammation, stabilizes the wound area, and supports smoother healing.
- Diabetic Foot Ulcers – Can support healthy circulation under clinical guidance.

Read more about Compression Therapy
Benefits of Compression Therapy
- Faster wound healing through improved circulation
- Reduced risk of recurrence, especially in venous ulcers
- Lower pain and discomfort due to decreased swelling
- Better mobility and overall patient comfort
How to Use Compression Therapy Safely
- Ensure Proper Fit – Pressure must match clinical needs; too little is ineffective, too much can cause skin damage.
- Monitor the Skin Regularly – Watch for numbness, tingling, coldness, or unusual pain.
- Increase Pressure Gradually – Start with lower compression levels and increase slowly under clinical supervision.
When Compression Therapy Should NOT Be Used:
Avoid compression unless recommended by a clinician if the patient has:
- Poor arterial circulation
- Active infection at wound site
- Acute heart failure
- Severe peripheral arterial disease (ABI)
Always consult a healthcare professional before beginning or modifying compression therapy.
Best Practices for Better Healing
Compression works best when combined with:
- Gentle wound cleansing
- Moisture-balancing dressings (foam, antimicrobial)
- Adequate nutrition (protein, vitamins, minerals)
- Regular assessments by wound-care specialists
Together, these steps create a complete, supportive healing environment.
Compression therapy is vital for accelerated wound healing, edema control, venous ulcer management, lymphedema care, and post-surgical recovery. When combined with appropriate dressings and monitored safely, it offers faster healing, improved patient comfort, and reduced risk of complications or recurrence.
Explore Professional Wound-Care Solutions – Wound Care Category

Nutrition plays a central role in wound healing, often as important as medical care itself. When the body sustains an injury, foods for wound healing become essential as its demand for specific nutrients increases.
The right foods can help accelerate tissue repair, reduce inflammation, strengthen the immune system, and enhance overall recovery. This blog explores scientifically backed foods for wound healing that actively support faster and more effective recovery.
Phytonutrient Power for Tissue Repair
What they are:
Phytonutrients are bioactive compounds in plants, such as flavonoids and carotenoids.
Why they matter:
Wound sites often experience oxidative stress due to free radicals, which can delay healing. Phytonutrients neutralize these free radicals, creating a favorable environment for tissue regeneration.
Food sources:
- Berries (flavonoids): Blueberries, strawberries, and blackberries reduce oxidative stress.
- Sweet potatoes & carrots (carotenoids): Support cell growth and boost skin barrier function.
Quick Tip: Including a cup of mixed berries in breakfast or roasted sweet potato as a side dish provides antioxidant protection during recovery.
Collagen-Activating Foods
What they are:
Nutrients that directly stimulate collagen synthesis.
Why they matter:
Collagen forms the structural framework of new tissue and strong scar formation.
Key nutrients & foods:
- Vitamin C (bell peppers, citrus, kiwi): A co-factor in collagen production.
- Copper (sunflower seeds, cashews, lentils): Supports the cross-linking of collagen fibers for durability.
Quick Tip: A salad of bell peppers, spinach, and sunflower seeds supplies both vitamin C and copper—maximizing collagen activation.
Gut Health and Healing Connection
What it is:
The gut microbiome plays a central role in nutrient absorption and immune regulation.
Why it matters:
Without a healthy gut, even the best diet cannot deliver full healing benefits. Probiotics strengthen the microbiome, enhance nutrient uptake, and improve immune defenses against infection.
Food sources:
Yogurt, kefir, kimchi, sauerkraut, miso.
Quick Tip: Consuming a serving of probiotic yogurt daily can improve nutrient bioavailability, indirectly accelerating wound recovery.
Anti-Inflammatory Spice Cabinet
What they are:
Natural spices with anti-inflammatory and antimicrobial properties.
Why they matter:
Chronic inflammation around a wound can slow tissue regeneration. Certain spices actively reduce inflammatory responses while fighting harmful microbes.
Food sources:
- Turmeric (curcumin): Reduces pro-inflammatory cytokines.
- Ginger: Enhances circulation and reduces swelling.
- Garlic: Provides antimicrobial support against infections.
Quick Tip: Adding turmeric to curries, ginger to tea, and garlic to meals integrates these benefits naturally into daily cooking.
Zinc Synergy Foods
What it is:
Zinc is essential for cell division and repair, but its efficiency increases when paired with vitamin C.
Why it matters:
Zinc deficiency can delay wound closure. Pairing zinc with vitamin C optimizes collagen production and tissue healing.
Food sources & pairings:
- Pumpkin seeds + oranges
- Chickpeas + bell peppers
This nutrient synergy ensures better absorption and function.
Iron-Rich for Oxygen Delivery
What it is:
Iron is critical for hemoglobin formation.
Why it matters:
Adequate hemoglobin ensures oxygen supply to regenerating tissues, which is vital for energy production during healing.
Food sources:
- Heme iron (easily absorbed): Red meat, chicken, fish.
- Non-heme iron: Lentils, spinach, fortified cereals.
Quick Tip: Pairing spinach (iron) with tomatoes (vitamin C) improves absorption, ensuring more oxygen reaches healing tissues.
Hydration Beyond Water
What it is:
Cellular hydration requires more than water—electrolytes are equally vital.
Why it matters:
Dehydrated cells cannot repair efficiently. Electrolytes maintain fluid balance, nerve signaling, and nutrient transport.
Food sources:
- Coconut water: Natural electrolytes.
- Watermelon & cucumbers: High water content plus minerals.
- Broths & soups: Provide both fluids and electrolytes.
Quick Tip: Including hydrating foods alongside water intake supports optimal tissue repair.
Building a Healing Plate
Recovery requires more than a single “superfood.” It’s about creating a balanced plate with antioxidant-rich phytonutrients, collagen -activating nutrients, probiotics, anti-inflammatory spices, zinc and iron synergy, and hydration strategies.
Together, these foods give your body the fuel it needs to rebuild stronger tissue, reduce complications, and support a faster recovery.
Take good care—and Happy Holidays! ❄️✨🎄

Living with diabetes means being extra vigilant about health, especially when it comes to wound care. Even minor cuts or blisters can progress into serious complications due to delayed healing, poor circulation, and increased infection risks.
This makes wound care a crucial part of diabetes management. Fortunately, modern solutions and advanced therapies are transforming the way patients and caregivers approach diabetic wound care.
1. Unique Challenges in Diabetic Wound Healing
Diabetic wounds differ from ordinary wounds in several ways:
- Reduced Sensation (Neuropathy): Many patients experience nerve damage that diminishes their ability to feel pain, making them less likely to notice small injuries.
- Impaired Circulation: Restricted blood flow slows the delivery of oxygen and nutrients essential for healing.
- Higher Infection Risk: Elevated glucose levels provide a favorable environment for bacteria, increasing the chance of infections.
Together, these challenges often lead to delayed healing and chronic wounds, particularly on the feet, making proactive care essential.
2. Innovative Wound Care Management Therapies
Recent advancements in wound care are improving recovery outcomes for diabetic patients:
- Velvert® Dressings: Designed to create a protective, moist healing environment that accelerates tissue repair.
- Negative Pressure Wound Therapy (NPWT): Uses gentle suction to remove fluids, reduce swelling, and promote faster healing.
- Hydrogel & Advanced Dressings: Maintain moisture balance, reduce pain, and minimize scarring.
- Antimicrobial Solutions: Dressings infused with silver or other agents help fight infection while supporting recovery.
These modern therapies go beyond basic bandaging, offering targeted solutions that actively support healing.
3. Importance of Early Detection and Timely Intervention
For diabetic patients, time is critical in wound management:
- Regular Self-Checks: Inspecting feet and legs daily for cuts, blisters, or redness.
- Professional Screenings: Routine check-ups with a podiatrist or healthcare provider.
- Prompt Action: Treating even minor wounds immediately with proper cleaning and dressings.
Catching a wound early can prevent it from progressing into a serious ulcer or infection that might require advanced medical intervention.
4. Integrating Preventive Care into Daily Life
Prevention is the cornerstone of diabetic wound care. Patients can reduce risks by adopting these practices:
- Daily Foot Inspections: Use a mirror or ask for assistance if needed.
- Skin Hydration: Keep skin moisturized to prevent cracks that can invite infections.
- Balanced Nutrition: A diet rich in protein, vitamins, and minerals supports healing.
- Protective Footwear: Always wear well-fitted shoes and socks to avoid friction and injury.
Incorporating these habits into daily routines ensures long-term protection.
5. Advanced Off-Loading Solutions
Pressure management plays a vital role in diabetic wound care:
- Total Contact Casting (TCC): Distributes weight evenly to reduce pressure on ulcers.
- Customized Diabetic Footwear: Specially designed shoes help minimize friction and pressure points.
- Pressure-Redistribution Insoles: Offer cushioning and support for patients with high-risk areas.
These solutions are critical for patients with foot ulcers, as they significantly reduce the chances of wound recurrence.
Empowering Diabetic Patients for Better Outcomes
Effective wound care is not just about healing—it’s about prevention, protection, and empowerment. By combining early detection, preventive strategies, advanced therapies, and innovative off-loading solutions, diabetic patients can significantly lower their risk of complications. With proactive care and modern tools, living with diabetes no longer has to mean living with chronic wounds.

