Diabetes significantly increases the risk of developing chronic wounds, particularly foot ulcers. Effective wound care is crucial for preventing complications and promoting healing in diabetic patients. In this blog, you will explore the nature of diabetic wounds, prevention techniques, and management strategies to help healthcare professionals and patients navigate these challenges.
Understanding Diabetic Wounds
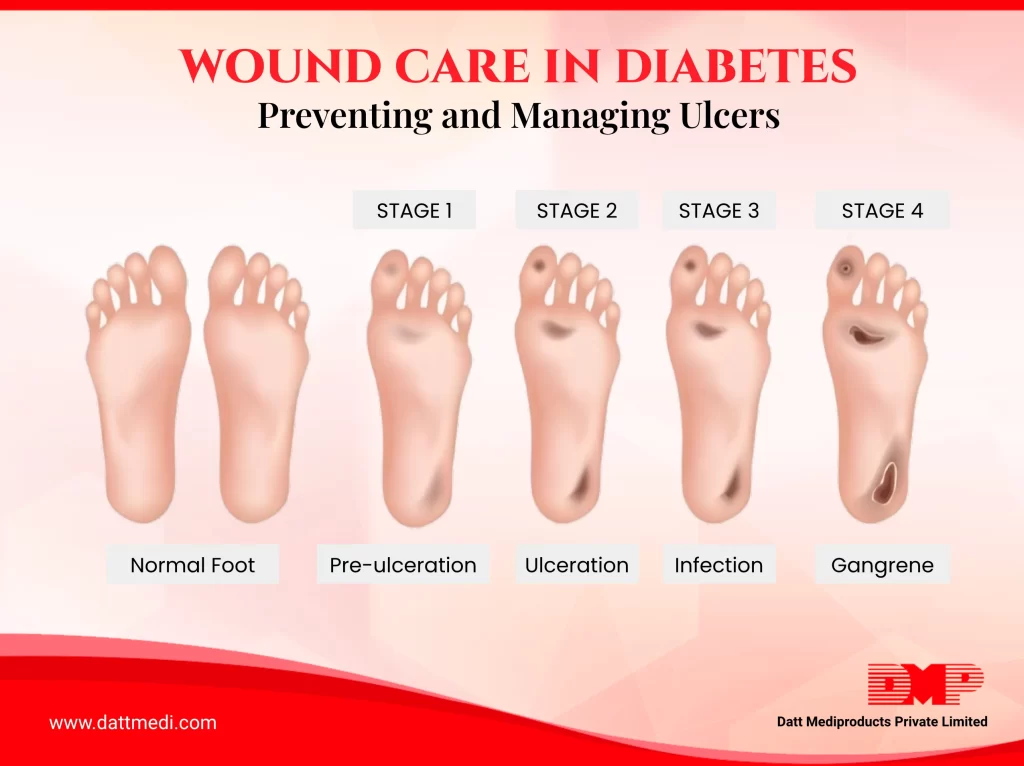
Diabetic wounds, especially foot ulcers, are common complications resulting from prolonged high blood sugar levels. These wounds often develop due to neuropathy (nerve damage) and peripheral arterial disease, which impair sensation and blood flow. Consequently, minor injuries can go unnoticed and progress into serious ulcers. Left untreated, these ulcers can lead to severe infections and, in extreme cases, amputations.
1. Prevention Techniques for Diabetic Ulcers:
Preventing diabetic ulcers is essential to reduce the risk of severe complications. Here are some effective prevention strategies.
2. Regular Foot Inspections:
Diabetic patients should inspect their feet (or have someone inspect it) on a daily basis for cuts, blisters, redness, or swelling. Early detection of potential issues can prevent minor problems from becoming serious ulcers.
3. Proper Footwear:
- Wearing well-fitting shoes and socks designed for diabetics can prevent pressure points and reduce the risk of injuries.
- Avoid wearing tight stockings or socks with elastic tops as they can reduce blood flow.
- Avoid extreme hot or cold temperatures.
- Do not treat corn or calluses on your own.
- Avoiding barefoot walking, even at home, is crucial.
4. Good Hygiene:
Keeping feet clean and dry is essential. Patients should wash their feet daily with mild soap and water, then dry them thoroughly, especially between the toes.
5. Blood Sugar Control:
Maintaining optimal blood sugar levels through diet, exercise, and medication can significantly reduce the risk of neuropathy and poor circulation, which contribute to ulcer formation.
6. Regular Medical Foot Check-Ups:
Routine visits to a healthcare provider or a podiatrist for foot exams can help identify and address problems early.
7. Management Strategies for Diabetic Patients:
When ulcers do occur, effective management is vital to promote healing and prevent complications.
Here are some key strategies:
- Wound Cleaning and Dressing: Keeping the ulcer clean and protected is essential. Cleaning the wound with a saline solution and using appropriate dressings, such as those provided by DMP Velvert®, can create an optimal healing environment. It provides a barrier to external contaminants, aids absorption of exudates and accelerates wound healing.
- Debridement: Removing dead tissue from the wound (debridement) can accelerate the healing process. This procedure should be performed by a healthcare professional.
- Pressure Offloading: Reducing pressure on the affected area is crucial. Patients may need special footwear, casts, or braces to alleviate pressure on the ulcer. Foot or mobility exercises also help in decreasing peak pressure, increasing foot and ankle range of motion and it improves neuropathy symptoms.
- Infection Control: Monitoring for signs of infection and using antibiotics when necessary is critical. Proper wound care products, like Velvert®, which offer antimicrobial properties, can help prevent infections.
- Blood Flow Improvement: Enhancing blood circulation through medical treatments or lifestyle changes can aid in the healing process. This might include medications, physical therapy, or surgical interventions. Revascularization results in increased tissue perfusion, which can further reduce amputation rates.
Diabetic ulcers are a serious complication of diabetes, but with proper prevention and management strategies, their impact can be significantly reduced. Regular foot inspections, good hygiene, appropriate footwear, and effective blood sugar control are key preventive measures. When ulcers do develop, it is best to catch them in the early stages when they are small, products combined with professional medical care, can promote healing and prevent complications.
At Datt Mediproducts, we offer Velvert®, an advanced wound care solution designed to aid in the management of diabetic ulcers. Velvert® dressings are crafted to provide superior moisture retention and protection, creating an optimal environment for wound healing. They also incorporate antimicrobial properties to reduce the risk of infection, which is crucial for diabetic patients. Velvert® is easy to apply and remove, ensuring minimal discomfort for patients.




