Wound healing is often slowed when the body cannot efficiently move blood and excess fluid away from the affected area. This causes low blood flow which leads to reduced oxygen & nutrient supply, both are critical for cell repair. This is frequently seen in chronic venous ulcers, lymphedema, diabetic wounds, and post-surgical swelling.
Compression therapy is one of the most effective clinical methods to improve circulation, support healing, and enhance overall wound management.
By applying controlled and consistent pressure, compression therapy reduces fluid buildup, improves oxygen delivery, and creates a stable environment that promotes faster tissue repair.
What Is Compression Therapy? How It Works
Compression therapy uses medical tools such as compression bandages, garments, or dressings to apply even pressure to a limb or wound site. This helps to:
- Redirect blood flow toward the heart
- Reduce fluid accumulation under the skin
- Improve oxygen supply to damaged tissues
- Support formation of healthier new tissue
This controlled pressure creates a stable, balanced healing environment and reduces strain on surrounding skin.
Types of Compression Therapy
1. Elastic Compression Bandages
Widely used for venous ulcers and chronic wounds because they allow adjustable pressure and support daily wound care.
Related Product: Compression Bandages – Wound Care Range
2. Compression Garments
Ideal for long-term swelling, lymphedema care, and post-surgical recovery. They offer uniform pressure and help maintain inflammation control. Velcare® Varicose Vein Stockings– Compression Garments
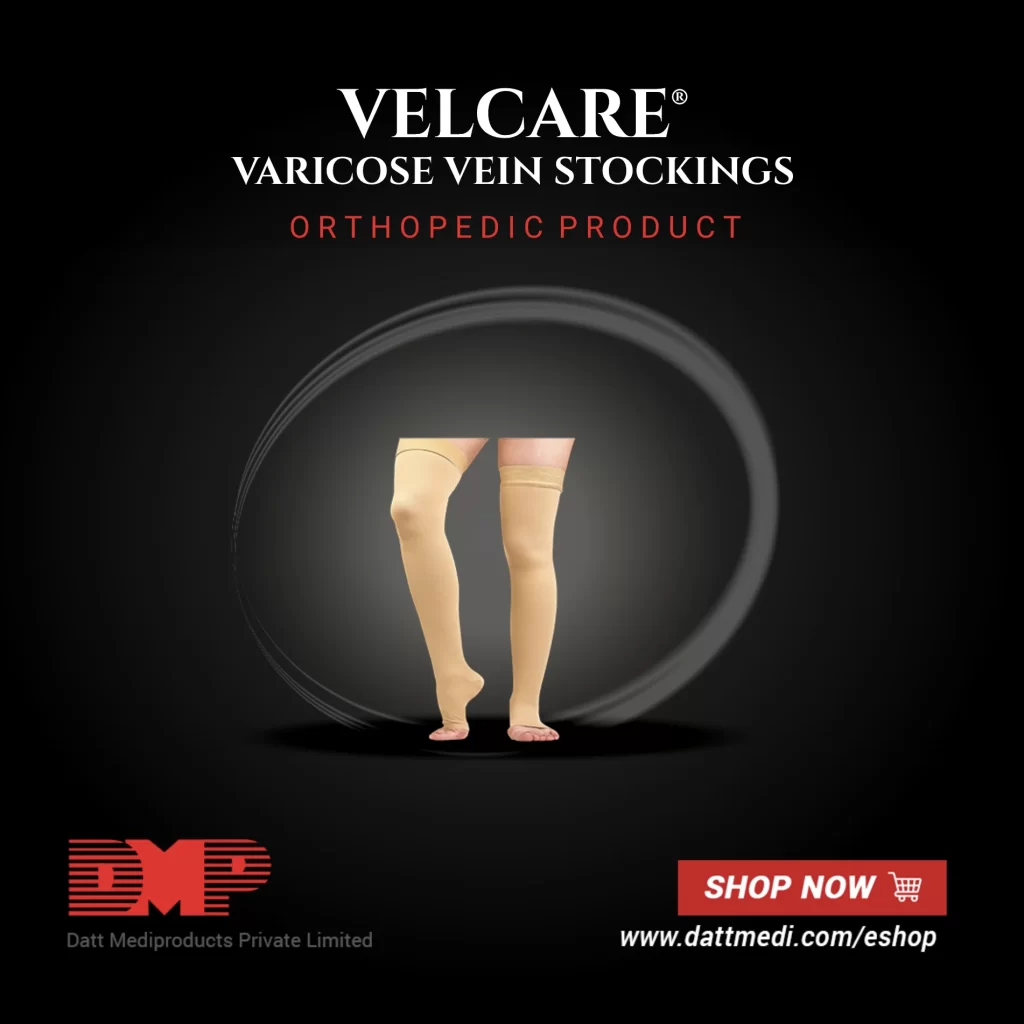
Know More About – Velcare® Varicose Vein Stockings- Compression Garments
3. Dressings With Built-In Mild Compression
Foam and hydrocolloid dressings provide gentle compression while maintaining moisture balance. Recommended options:
- Velfix® Foam Dressings – Advanced Wound Care
- Velsoft® Silicone Foam Dressings – Advanced Wound Care
- Velvert® Advanced Dressings – Antimicrobial & Moisture Management
How Compression Therapy Supports Wound Healing
- Improved Blood Flow – Prevents blood pooling and delivers oxygen and nutrients for efficient tissue repair.
- Swelling Control (Edema Management) – Removes trapped fluid, reducing discomfort and creating a stable environment.
- Enhanced New Tissue Formation – Supports orderly tissue repair and faster wound closure.
- Reduced Risk of Raised Scars – Mild compression after surgery or burns helps prevent thick or raised scars.
When Compression Therapy Is Recommended
- Chronic Venous Ulcers – Supports circulation and long-term healing.
- Lymphedema Care – Manages fluid buildup, heaviness, and infection risk.
- Post-Surgical Recovery – Controls inflammation, stabilizes the wound area, and supports smoother healing.
- Diabetic Foot Ulcers – Can support healthy circulation under clinical guidance.

Read more about Compression Therapy
Benefits of Compression Therapy
- Faster wound healing through improved circulation
- Reduced risk of recurrence, especially in venous ulcers
- Lower pain and discomfort due to decreased swelling
- Better mobility and overall patient comfort
How to Use Compression Therapy Safely
- Ensure Proper Fit – Pressure must match clinical needs; too little is ineffective, too much can cause skin damage.
- Monitor the Skin Regularly – Watch for numbness, tingling, coldness, or unusual pain.
- Increase Pressure Gradually – Start with lower compression levels and increase slowly under clinical supervision.
When Compression Therapy Should NOT Be Used:
Avoid compression unless recommended by a clinician if the patient has:
- Poor arterial circulation
- Active infection at wound site
- Acute heart failure
- Severe peripheral arterial disease (ABI)
Always consult a healthcare professional before beginning or modifying compression therapy.
Best Practices for Better Healing
Compression works best when combined with:
- Gentle wound cleansing
- Moisture-balancing dressings (foam, antimicrobial)
- Adequate nutrition (protein, vitamins, minerals)
- Regular assessments by wound-care specialists
Together, these steps create a complete, supportive healing environment.
Compression therapy is vital for accelerated wound healing, edema control, venous ulcer management, lymphedema care, and post-surgical recovery. When combined with appropriate dressings and monitored safely, it offers faster healing, improved patient comfort, and reduced risk of complications or recurrence.
Explore Professional Wound-Care Solutions – Wound Care Category