Choosing the Right Dressing for Chronic Wounds
Chronic wounds, such as diabetic ulcers, pressure sores, and venous leg ulcers, present unique challenges in wound care management. These wounds often resist healing due to underlying conditions such as poor circulation, increased infection risks, prolonged or excessive inflammation, and other patient-specific factors.
Selecting appropriate dressings tailored to the needs of chronic wounds is essential to promote healing and prevent complications.
Chronic wounds develop due to systemic issues that delay natural healing. Common types include:
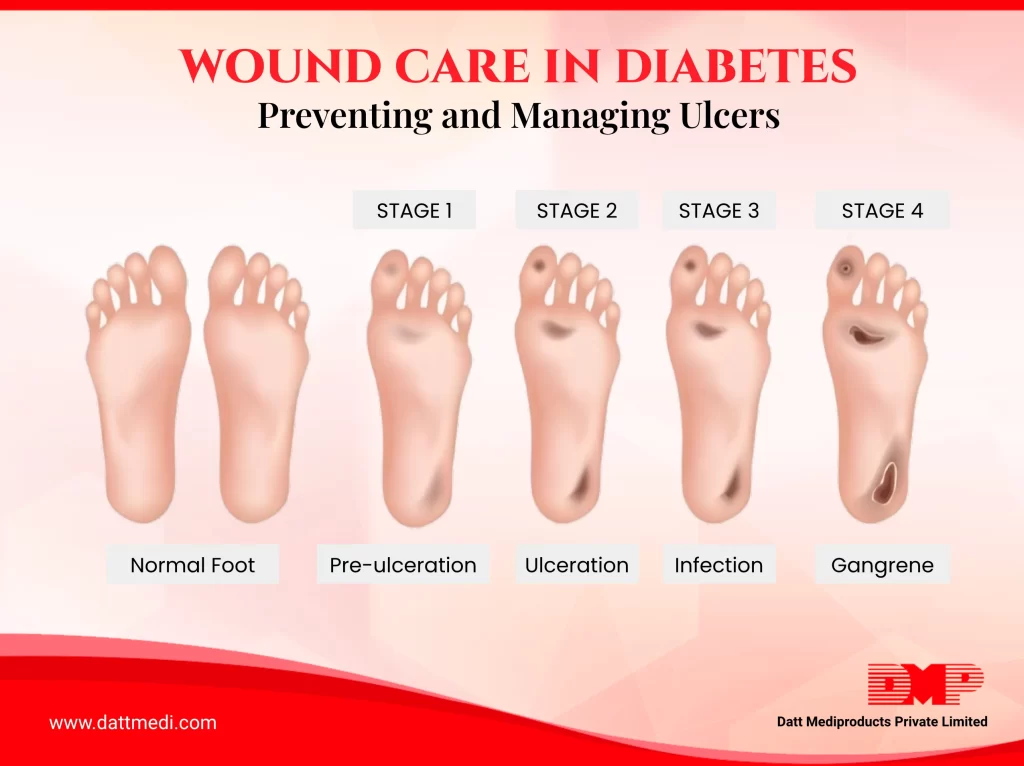
- Diabetic Ulcers: These ulcers result from reduced blood flow and nerve damage, often occurring on the feet. Proper care involves maintaining a balance between moisture and dryness, ensuring the wound does not become too dry or overly moist.
Stat Spotlight
In India, diabetic foot ulcers account for approximately 20% of all diabetes‑related hospitalizations. ~ Source
- Pressure Sores: Caused by prolonged pressure on the skin, these wounds are common among bedridden or immobile patients. Managing pressure and ensuring the wound stays clean and protected are vital.
Stat Spotlight
In India, point‑prevalence studies report that approximately 5% of hospitalized patients have pressure ulcers, underscoring the importance of preventive care. ~Source
- Venous Leg Ulcers: These ulcers result from chronic venous insufficiency, in which impaired venous return causes fluid to accumulate in the lower legs, increasing tissue pressure and leading to skin breakdown. Effective management typically centers on graduated compression therapy to improve circulation, alongside advanced dressings to control exudate, leg elevation, and skin care to protect the periwound area.
Managing these wounds involves addressing infection risks, ensuring patient comfort, and promoting effective healing using evidence-based dressing solutions. Selecting the appropriate dressing depends on the type of wound, its condition, and the specific challenges it presents.
Below are some general guidelines:
Diabetic Ulcers
Dressings should maintain moisture balance and provide effective infection control. Non-adhesive dressings are preferred to minimize skin damage during dressing changes. Velvert®, with its strong antimicrobial properties and excellent moisture management, is ideal for diabetic ulcers and wounds at high risk of infection.
Pressure Sores
These wounds require dressings that redistribute pressure and effectively manage exudate to prevent further tissue damage and support healing. Velfix®-S offers both cushioning and absorption, making it a reliable choice for pressure sores and wounds requiring enhanced comfort and protection.
Venous Leg Ulcers
Advanced dressings used in combination with compression therapy are essential for managing exudate and improving circulation. Velfour®, with its high absorption capacity, is well-suited for heavily exuding wounds, including venous leg ulcers.
Infected Wounds
Antimicrobial dressings are effective in managing bacterial growth and reducing the risk of complications. Silvel™ with its strong silver based antimicrobial action and Velvert™ with their strong silver-based antimicrobial action, are suitable for infected or high-risk wounds such as second-degree burns, necrotizing fasciitis, and traumatic wounds.
Here are some types of advanced dressings that address specific wound care needs:
Antimicrobial Dressings
Designed to manage infection risks, these dressings often contain agents like silver to inhibit bacterial growth. Silvel™ and Velvert™ are widely used for diabetic ulcers and pressure sores prone to infection, owing to their strong antimicrobial properties.
Foam Dressings
Highly absorbent, these dressings are ideal for wounds with significant exudate, such as venous leg ulcers. They also offer cushioning to enhance patient comfort. Velsap™ and Velfix®-S are designed for moderate to heavily exuding wounds, ensuring effective fluid management and reduced dressing change frequency.
Multi-Layer Dressings
These dressings provide both absorption and protection, making them effective for managing pressure sores and heavily exuding wounds. Velfour® is an excellent example, offering essential support for such wound types.
Real-Life Example
A 60-year-old diabetic patient in India developed a non-healing foot ulcer. Initially, traditional gauze dressings were used, leading to frequent infections. After switching to Velvert™ antimicrobial dressing, the wound showed significant improvement within four weeks, with reduced exudate and no further infections. This case highlights the importance of selecting the right dressing for chronic wounds.
Practical Tips for Managing Chronic Wounds
Effective wound care goes beyond dressing selection. Here are additional strategies to optimize healing:
- Proper Cleaning and Debridement: Regularly cleaning the wound and removing dead tissue helps create an optimal environment for healing.
- Adjunctive Therapies: Techniques like compression therapy for venous ulcers and offloading for diabetic foot ulcers can significantly improve outcomes.
- Regular Monitoring: Chronic wounds require consistent evaluation to identify changes in size, depth, or signs of infection, allowing timely adjustments in care.
- Consulting Professionals: Work with healthcare providers to ensure the care plan addresses the wound’s unique needs and aligns with the patient’s overall health condition.
Selecting the right dressing for chronic wounds can significantly improve healing outcomes and enhance patient comfort. By understanding wound characteristics and tailoring treatments accordingly, healthcare professionals can address even the most challenging cases effectively.